Abstract
Introduction: Myelodysplastic neoplasms (MDS) are clonal disorders of relative bone marrow failure and a variable risk of progression to acute myeloid leukemia. MDS generally exhibit genetic and/or cytogenetic abnormalities, an observation that led to the reclassification of MDS in the World Health Organization (WHO) 2022 update (Khoury et al, Leukemia 2022). In parallel, studies examining the mutational landscape of MDS have shown that specific patterns of somatic gene alterations strongly impact prognosis (Bernard et al, NEJM Evidence, 2022). In this study, we characterized the mutational patterns and clinical outcomes associated with the WHO 2022 classification schema to provide a more comprehensive view of this disease framework.
Methods: This is a single-center retrospective cohort study of patients (pts) with clinicopathologically-confirmed MDS between January 2018 and December 2021. We identified cases with next-generation sequencing (NGS) performed on either bone marrow (BM) aspirate or peripheral blood (PB) using a clinically validated 164 gene panel designed to detect genes recurrently mutated in both myeloid and lymphoid neoplasms. For all cases, demographic information, clinical and molecular data, WHO 2022 diagnostic class, and survival outcomes were collected. IPSS-R and IPSS-M scores were calculated. Survival was estimated using the Kaplan-Meier method. Comparisons of mutational frequencies between groups were made via Fisher's exact test. This study was approved by Stanford University's Institutional Review Board.
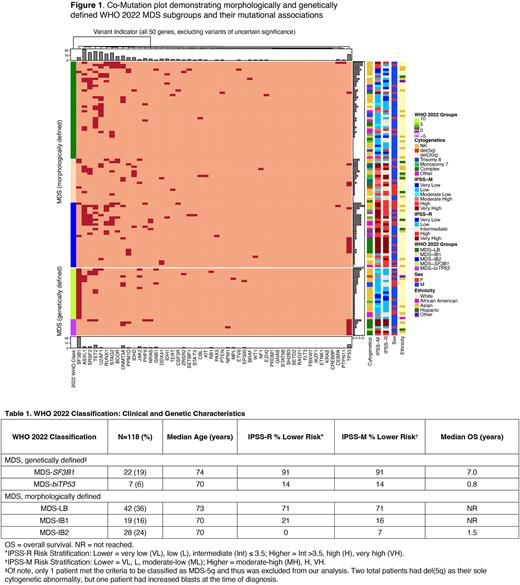
Results: Our inclusion criteria identified 118 MDS pts with clinicopathologic and molecular review. The median age of the cohort was 72 years, 67% were male, and 70% were Caucasian. For morphologically defined pts, MDS with low blasts (MDS-LB) was the most common subtype (36% of the entire cohort), followed by MDS with increased blasts-2 (MDS-IB2; 24%) and MDS with increased blasts-1 (MDS-IB1; 16%). For genetically defined pts, MDS with low blasts and SF3B1 mutation (MDS-SF3B1) was the most common subtype (19%) while MDS with biallelic TP53 mutations (MDS-biTP53) comprised 6% pts (Table 1). Within the latter group, 86% had a complex karyotype.
A co-mutation plot to visualize the distribution of mutations among the various subgroups is shown in Figure 1. Notably,TP53 mutations (either mono- or bi-allelic) occurred in 16% of the cohort, were frequent in pts with complex karyotype (17/22; 77%), and were exclusive of ASXL1, IDH2, or SF3B1 mutations. In the morphologically defined subgroups, pts with MDS-LB had the highest prevalence of TET2 mutations (12/42 pts; 29%), while pts with MDS-IB1 had none (0/19 pts). U2AF1 mutations were significantly more common in pts with MDS-LB (13/42; 31%) relative to pts with MDS-IB2 (2/28; 7%) (p = 0.04). Conversely, patients with MDS-IB2 more frequently harbored TP53 mutations compared to pts with MDS-LB (p = 0.002).
Calculation of IPSS-M scores stratified 47% of pts into the lower risk categories, with the remainder in higher risk categories (Table 1). The median IPSS-M score for the entire cohort was 0.105 [min: -2.11, max: 4.59] (Moderate High, MH). Median IPSS-M scores were highest in pts with MDS-biTP53 (3.18; [-0.480, 4.59]) and MDS-IB2 (1.65; [-0.880, 3.47]) (Very High, VH), and lowest in pts with MDS-SF3B1 (-1.13; [-2.06, 0.250]). IPSS-R scores generally paralleled IPSS-M scores, with 46% of all pts falling into the lower risk groups (Table 1). Pts with MDS-biTP53 had a median IPSS-R score of 8.0 [3.0, 9.5] (VH) while pts with MDS-SF3B1 had a median score of 2.5 [1.5, 4.0] (MH).
Median overall survival (mOS) from the time of diagnosis was highest for those with MDS-LB (not reached), MDS-IB1 (not reached), and MDS-SF3B1 (7.0 years). Survival for patients with MDS-IB2 and MDS-biTP53 was poor, with mOS of 1.5 years and 0.8 years, respectively (Table 1).
Conclusion: Our data demonstrated the clinical and molecular characteristics of MDS pts evaluated within the WHO 2022 schema and showed that differing mutational features were prominently associated within the morphologically as well as the genetically defined subgroups. Further, OS differed substantially among the defined subgroups. Our incorporation of the IPSS-M and IPSS-R provides additive prognostic and survival components into the WHO 2022 classification, which together enhance this framework's utility for studying MDS and its natural history.
Disclosures
Fernandez-Pol:Cartography Biosciences: Consultancy; Leica Biosystems: Ended employment in the past 24 months, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal