Abstract
Introduction: High-intensity therapeutic regimens results in ALL have not been reproduced in limited resource settings, due to the lack of appropriate support therapy, diagnostic methods, limited access to drugs, and high treatment related mortality. For low and middle-income countries, treatment of these patients represents a challenge. In Mexico acute leukemia represents 49% of all pediatric cancers, with a 5-year overall survival between 50 and 60%, a relapse rate of 26%, induction related mortality of 3-10%, and a mortality in remission of 14%.
We report the results of an adjusted treatment regimen based on an adapted risk stratification for a limited-resource setting.
Objective: To implement a risk stratified treatment protocol for a limited resource setting, with the aim of reducing induction related mortality, and improving EFS and OS.
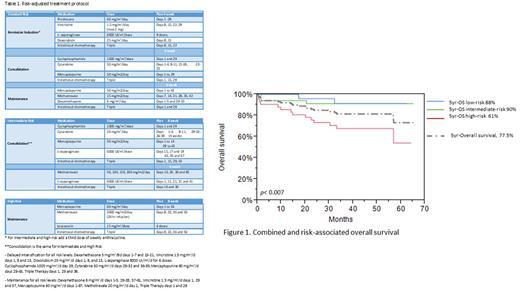
Materials and Methods: From January 2017 to March 2020, all patients diagnosed with ALL between 0 and 15 years of age in a single center in northeast México were captured in a prospectively maintained database. Depending on risk stratification, patients received an adjusted treatment protocol with variations on intensity and duration for the different phases. The main differences were the amount of anthracycline doses during induction (2 for low, 3 for intermediate/high patients), the requirement of at least 20 doses of L-asparaginase for intermediate/high risk patients, and the use of Capizzi-style methotrexate for intermediate risk and high-dose methotrexate only for high-risk patients (Table1). Demographic data was reported using distribution analysis, and the Kaplan-Meier method was used to analyze and predict OS and EFS.
Results: There were 59 male and 41 female patients; the median age at diagnosis was 5.5 years. B-cell and T-cell lymphoblastic leukemia was the diagnosis in 94% and 6% patients, respectively, with a follow-up of 41 (0.33-65) months. Regarding risk stratification, 42%, 34%, and 24% children were classified as high, intermediate, and low-risk, respectively. After one week of corticosteroids 80% of patients had a good response, and 84% of patients achieved a negative measurable residual disease (MRD) after induction chemotherapy.
Estimated EFS and OS at 5 years were 70% and 77.5% respectively. Of the 93 patients evaluable for response, MRD positivity (16%), induction related mortality (6%), and relapse (16%) rates were lower in this cohort when contrasted with previous protocols. EFS for low, intermediate, and high-risk groups was 73%, 85%, and 56% and OS 88%, 90% and 61% (Figure 1)
Conclusions: The implementation of a risk-adjusted chemotherapy regimen adapted for our limited-resource center, improved treatment continuity and was associated with better OS, and EFS. Early relapse rates were also reduced, without increasing induction mortality associated with toxicity.
Periodic and prospective outcome evaluation in a limited-resource setting is fundamental to adjust and standardize therapy.
Disclosures
Gómez-De León:AbbVie: Honoraria, Other: advisory board. Gómez-Almaguer:Janssen: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; BMS: Consultancy, Honoraria. Gonzalez:AMGEN: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal