Abstract
Background: Tandem CD19/CD20 CAR T cells, which got two scFvs connected to a single molecule with different antigen specificities simultaneously, not just showed broad antigen coverage, yet additionally had robust antitumour activity in vitro. The best overall response rate was 78% with 70% achieving a CR. Here, we report updated clinical outcomes from this trial.
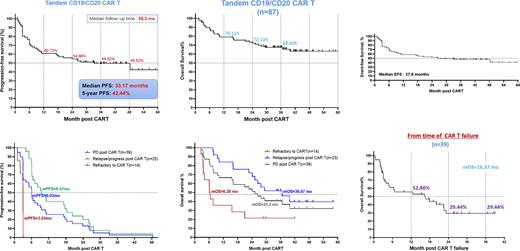
Methods: 87 patients with R/R B-NHL after ≥ 2 lines of therapy (including an anti-CD20 mAb plus an alkylating agent) recruited between 2017.05 and 2020.01, which underwent leukapheresis and conditioning chemotherapy followed by a Tandem CD19/CD20 CAR T cells at doses of 0.5 - 8×106/kg of body weight. The updated follow-up analysis was mainly in median PFS, median OS, and median EFS. Besides, survival status of patients after CAR T failure were also observed in the follow-up data.
Results: Up to 2022.5.10, the median follow-up time was 38.3 months, 40 patients (45.98%) still keep ongoing response, and the median PFS was 33.17 months, with 49.52% of 3-year PFS rate; the median EFS was 27.6 months, with 47.51% of 3-year EFS rate. The median OS was not reached, with 68.6% of 3-year OS rate. Nonrelapse mortality was 4.4%. Among 39 patients (44.83%) experienced PD after tandem CD19/CD20 CAR T infusion, best response was 54% CR and 10% partial response (PR); 36% were primary refractory, the median PFS was 6.03 months, and the median OS was 25.2 months. Survival data were statistically analysed for patients after CAR T failure, the median follow-up was 26.77 months , and the median OS was 16.37 months.
Conclusions: With 3-year follow-up, Tandem CD19/CD20 CAR T cells demonstrated substantial and continued benefits in patients with r/r B-NHL. High CR rates lead to sustained remission and durability, with a long-term median PFS and high percentage of patients in ongoing response at data cutoff, maintained a manageable safety profile, with no new safety signals. For the patients failure after tandem CD19/CD20 CAR T treatment, other anti-tumor regimens, such as bispecific antibodies, target drugs, immunomodulator, secondary CAR T, radiotherapy and so on, could also appeared to attain efficacy outcomes to improve these patient's survival.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal