Abstract
Background: Older adults with AML have a decline in performance statues and acquired comorbidities compared to younger patients. Treatment intensity and outcomes were varied according to those factors. Various studies tried to classify genetic landscapes to predict outcomes in AML patients. However, those were mostly for younger patients treated with intensive chemotherapy. Machine learning (ML) is useful for classifying large data by calculating each data and subtracting characteristics. Given the limited data of genomic classification for older adults with AML, we analyzed genetic landscapes using ML in the context of treatment intensity.
Methods: Unsupervised hierarchical clustering method was used to determine the most likely set of clusters according to cytogenetic/mutation properties at AML diagnosis. Patient selection criterion for this analysis were set as follows; (a) elderly (60 years or older) AML patients who were diagnosed in Seoul St. Mary's Hospital between Jul 2017 and Oct 2021, (b) having available information on chromosome and gene mutation at diagnosis and (c) treated with either intensive chemotherapy (IC), hypomethylating agents (HMA), or HMA plus Venetoclax (HMA/VEN). Patients who received best supportive care only were not included in this study.
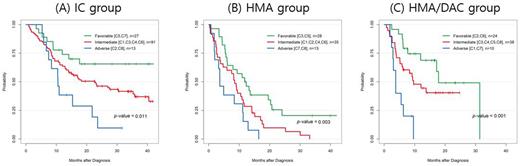
Results: A total of 279 patients who met inclusion criteria were selected and their median age at diagnosis was 68 years (range 60-). As first-line treatment, 131 patients received IC (47.0%), 76 patients received HMA only (27.2%), and 72 patients were treated with HMA/VEN (25.8%). After a median follow up of 22.5 months, the median overall survival (OS) in the three groups were 22.7, 8.8, and 12.0 months, respectively (p<0.001). We applied the ELN2022 risk stratification to these 3 different treatment groups. For IC group, there was no survival difference between favorable, intermediate, and adverse groups (44 months, 23.1 months, 14.9 months p=0.255). In addition, HMA groups (p-value =0.903) and HMA/VEN group (p-value = 0.805) did not showed survival differences according to risk groups by ELN2022.
Next, we conducted hierarchical clustering analysis in a total cohort, which was found to be best classified into 8 clusters by indices for determining the number of clusters. The dominant cytogenetic features of each cluster are demonstrated as follows. The cluster 1(C1) was a group that IDH1 and TP53 mutations were mostly proportioned; C2 was RNA splicing gene dominant (U2AF1 or SRFS2 mutations); C3 was ASXL1 and complex karyotype dominant; C4 was DNA methylation dominant (DNMT3A or TET2 mutations); C5 was NPM1 dominant; C6 was FLT3 mutations dominant; C7 was RUNX1-RUNX1T1 or CBFB-MYH11 fusion dominant; and C8 was abnormal karyotype [-5 or del(5q); -7;-17/abn(17p)] dominant. Thereafter, we linked these genomic clusters with survival outcomes of each treatment arm. Among the 131 patients in the IC group, C5 and C7 were identified as favorable groups while C2 and C8 were classified as adverse groups. On the other hand, in the HMA group, C3 and C5 were allocated to favorable groups and C7 and C8 as adverse. In the HMA/VEN group, C2 and C6 showed favorable survival outcomes while C1 and C7 showed poorer outcomes. Interestingly, we found that an allocation of each genomic cluster to three distinguished (favorable, intermediate, adverse) prognostic groups was changed by the treatment types and survival outcomes of each cluster was substantially different according to different treatment arms. The groups of C1, C5, and C7 which included the HMA/VEN adverse group showed no differences in OS between HMA and HMA/VEN groups, while IC showed better outcomes (HMA vs. HMA/VEN vs. IC, 9.6 vs 9.2 vs 40.5 months, p<0.001). Among the groups of C2, C4, C6, and C8, the patients showed similar median OS between intensive chemotherapy and HMA/VEN, but both treatments showed better outcomes than HMA only (HMA vs HMA/VEN vs IC, 5.5 vs 17.2 vs 17.4 months, p<0.001). In addition, groups C2 and C4 had better median survival by DAC/VEN therapy than other kinds of treatment. (HMA vs HMA/VEN vs IC, 8.2 vs 17.5 vs Not reached, p=0.039).
Conclusion: This study suggests that genomic clustering by unsupervised ML could identify genomic groups by co-occurrence patterns having different survival outcomes according to each treatment modality, thus potentially guiding treatment selection in older adults with AML.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal