Abstract
Venous thromboembolism (VTE) is a known complication of hospitalization for acute medical illness; hospitalized patients with cancer represent a particularly high thrombotic risk population. However, there is significant underuse of thromboprophylaxis in medical inpatients with cancer.
The objective of this study is to characterize the use of thromboprophylaxis in hospitalized patients with cancer at Windsor Regional Hospital (WRH), a large, community-based hospital in Ontario, Canada. Specifically, we investigated use of both pharmacologic and mechanical thromboprophylaxis, along with clinical determinants underlying lack of VTE prophylaxis to better understand our local practice patterns.
This study is a retrospective, single center cohort study of 120 adult patients admitted to WRH with a primary solid tumor diagnosis (n=57) and hematologic cancer diagnosis (n=63) over a 3-month period. Chart review was performed for the first ten days of admission or until discharge. Multi-variate analyses were employed to determine clinical predictors of thromboprophylaxis use.
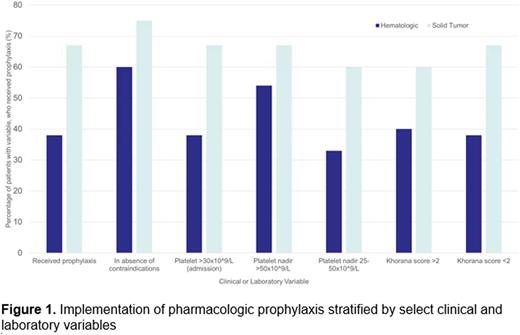
Sixty-one (51%) medical inpatients with cancer received pharmacologic thromboprophylaxis during their hospitalization. The majority of patients (n=39; 68.4%) with a solid tumor malignancy received prophylaxis, while only twenty-two (34.9%) patients with a hematologic malignancy were provided pharmacologic VTE prophylaxis. In the subgroup of patients without contraindications to pharmacologic prophylaxis, 60% of patients with a primary hematologic diagnosis and 75% of patients with a primary solid tumor diagnosis received pharmacologic prophylaxis (Figure 1). 4 of 58 patients who did not receive pharmacologic prophylaxis received mechanical prophylaxis during admission (6.9%). Risk of VTE stratified by Khorana score >2 or ≤2 was not associated with use of pharmacologic prophylaxis (p=0.255). Platelet nadir <25x109/L (OR=0.12, 95% CI 0.0256-0.4087), active hormonal therapy (OR=0.11, 95% CI 0.0055-0.6707) and pulmonary disease at baseline (OR=4, 95% CI 1.0031-22.9064) were the only patient variables significantly related to the odds of pharmacologic prophylaxis. Given the limited number of patients in the study with pulmonary disease and maintained on hormonal therapy at baseline, the statistical significance may not correlate to clinical significance.
In conclusion, thromboprophylaxis is an integral adjunct to the management of medical inpatients with active cancer yet is often neglected in clinical practice. In our population, nearly half of patients were not provided VTE prophylaxis. Severe thrombocytopenia and active hormonal therapy were negative predictors of pharmacologic thromboprophylaxis use while the presence of pulmonary disease favored prescription of prophylaxis on admission. Further studies are needed to better understand the rationale underlying omission of VTE prophylaxis in medical inpatients with cancer, and raise awareness of measures to prevent VTE in this patient population.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal