Abstract
The use of empiric broad-spectrum antibiotics for the treatment of febrile episodes during the first weeks of allogeneic transplant has been associated with an increase in the incidence of acute Graft versus Host Disease (aGVHD) and transplant-related mortality (TRM). However, there are several confounding factors; age, donor source, conditioning, GVHD prophylaxis, disease index risk, comorbidities, and the time of initiation of antibiotics that can preclude strong conclusion regarding the importance of this association. We present the outcomes of a cohort of 274 patients whose received or not antibiotics in the early phase of transplant after adjustment for confounding factors and competing risks
Methods and patients. Retrospective cohort study from a single cancer center. All consecutive patients older than 15 years and transplanted with bone marrow or peripheral stem cell, from Jan 2003 to Dec 2019, were included. The cohort who was exposed was composed of the patients that received IV antibiotics between day - 7 and + 7 and it was compared with the group that did not. TRM was defined as death due to any transplantation-related cause other than disease relapse from day 0 until + 365, aGVHD was diagnosed and classified according to MAGIC criteria and it was measured until d + 100. For statistical porpoises univariable and multivariate survival analyses were conducted, and Fine-Gray models were fitted to account for competing risks, also, an exploratory subgroups analysis was conducted according to the type of antibiotic received. The study was approved by Institutional Ethic Committee
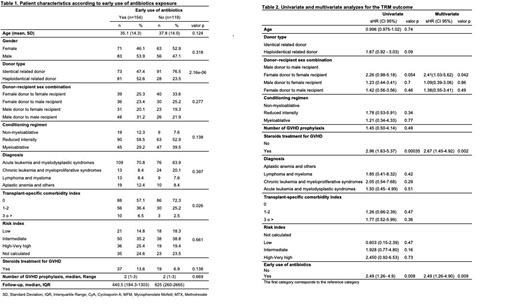
Results. The main characteristics of the patients are summarized in table 1. Briefly: the whole group consisted of 274 patients; median age 36.6 years, 244 had malignancies, 185 acute leukemia. The disease index risk was intermediate or higher in 250, 109 underwent to haplo transplant, and 150 received cyclophosphamide pos transplantation. 154 (56%) received early antibiotic and 119 (44%) did not. The median follow-up for the entire group was 560 days, the cumulative incidence (CI) of TRM at 1 year was 21% in the exposed group vs. 9% in the non-exposed p: 0.007. Without adjustment, early use of antibiotics was associated with a significant increase in the TRM risk (sHR 2.49, 95%CI: 1.26-4.9; p=0.008), and after adjustment, it continued to be an independent risk factor for TRM (sHR 2.48, 95%CI: 1.25-4.90; p=0.009) (table 2). The CI of aGVHD was 24% in the exposed patients vs.15% in the other group; p=0.049). Without adjusting, the early use of antibiotics was associated with an increase in the risk (sHR 1.74, 95%CI: 1.00-3.03; p=0.05), however, after adjusting in multivariate analysis, this effect did not persist (sHR 1.49, 95%CI: 0.818-2.73; p=0.19).
Regarding the antibiotic administered it was meropenem in 60% of the cases, cefepime in 30%, and vancomycin was added in 18%. When comparing each antibiotic with the non-early use of them, both, cefepime and meropenem were associated with increased risk of TRM (p=0.008 and p=0.003, respectively) while no differences were found between the use of vancomycin and the non-use of antibiotics (p:0.615)
Conclusion. This study shows that, after adjusting for several confounding factors and competing risk, the early use of antibiotics during allogeneic transplant increases the risk of TRM. This result is in concordance with those obtained by other groups which studied the effect of them in late periods of the transplant. However, our finding, in terms of aGVHD, is different from those which have been published, this is difficult to explain, and it is hypothesis generating; we can speculate that the use of post-transplant cyclophosphamide in an important part of our cohort, including sibling donors, and the low incidence of this complication in the whole cohort can be part of the explanation. Understanding whether GVHD is a mediator between antibiotic use and mortality requires further investigation. For a while, the results of this and other studies demand to be cautious with the use of empiric antibiotics during the early period of the allogeneic transplantation
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal