Abstract
Introduction:
Acute Lymphocytic Leukemia (ALL) is a malignancy of lymphocytes characterized by uncontrolled proliferation of immature cells which ultimately leads to the replacement of bone marrow and other lymphoid organs. Typically, ALL develops in a previously healthy person however, it can rarely progress from an existing Myelodysplastic syndrome (MDS) or Chronic Myeloid Leukaemia (CML). In this study, we highlight the baseline characteristics and outcomes in patients with ALL and previous diagnoses of MDS or CML.
Methodology:
Healthcare Cost and Utilization Project National Inpatient Sample (HCUP-NIS) was queried to identify all ALL admissions between 2016-2019 in adult patients with a secondary diagnosis of MDS or CML using International Classification of Disease 10th Revision (ICD-10) codes. We evaluated baseline characteristics including Age, Sex, Race, Insurance type, Median household income, Region of hospital, Hospital Bed size, and Location/teaching status of hospital, in addition to mortality as the primary outcome and length of the hospital stay (LOS) and total hospital charges (THC) as secondary outcomes.
Results:
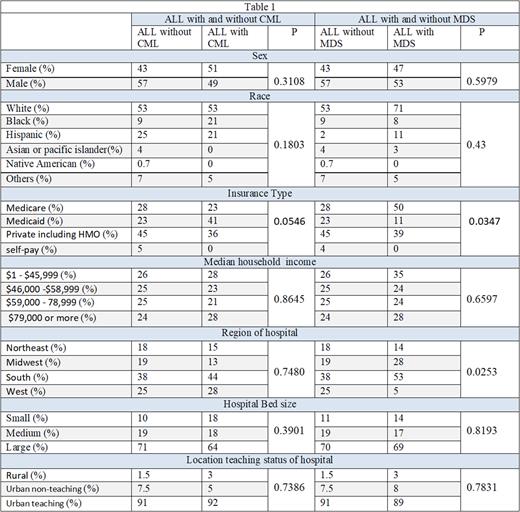
A total of 27385 patients with ALL were hospitalized and among them, 195 (0.7%) had a secondary diagnosis of CML. The mean age of the CML group was non-significantly higher (51.3 vs. 48.5) compared to those without CML. In patients with ALL and previous CML, there was a higher proportion of female sex, black race, Medicaid insurance, hospitalizations in south and west region, small sized hospitals in comparison to those with ALL without previous CML. though not statistically significant as reflected in Table (1). There was no difference in, Charlson comorbidity index, and household income. CML group had non-significantly lower odds of mortality in comparison to patients without CML (5.1% vs 5.8 % P=0.84) with adjusted odds ratio (AOR) of 0.79 (p=0.75 CI 0.18-3.34). Patients with a higher Charlson comorbidity index had significantly higher odds of mortality (1.68 with P=0.022). Among secondary outcomes, the CML group had a higher mean length of stay (20.3 vs 18) and lower THC ($240161 vs $279386) although this did not reach statistical significance.
Out of all patients admitted with ALL, 180 (0.6%) had a secondary diagnosis of MDS, and the mean age of the MDS group was higher (62.6 vs. 48.4) compared to the other group. In ALL patients with previous MDS group, there was a significantly higher proportion of people with Medicare insurance, and hospitalization in the south and west region. There was a trend towards an increased proportion of Female sex, white Race, lower median household income, small sized hospitals in comparison to ALL without previous MDS group though it was not statistically significant (Table1). Patients with ALL and a previous Diagnosis of MDS had non-significantly higher odds of mortality (11% vs 6 %) in comparison to patients without MDS (AOR 1.7 p=0.32 CI 0.60-6.65). Among the secondary outcomes, the MDS group had a non-significantly lower mean LOS (12 vs 18) and lower THC ($243389 vs $ 279112).
Conclusion:
In this analysis, we found that sex, race, insurance type, median household income, and region of the hospitalization impacts the risk of developing ALL after MDS or CML. Prospective studies are required to look into the cause of these differences as it can be related to the socioeconomic disparities or specific gene mutations more prevalent in certain races of regions.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal