Abstract
Introduction: Little is known of the relationship between myeloproliferative neoplasm (MPN) and sickle cell disease (SCD), possibly due to under diagnosis from symptom overlap. Few studies exist documenting cases of concomitant MPN in SCD patients, likely because the confounding presence of reactive thrombocytosis in SCD and masking of polycythemia in SCD making the diagnosis of essential thrombosis (ET) and polycythemia vera (PV) difficult.
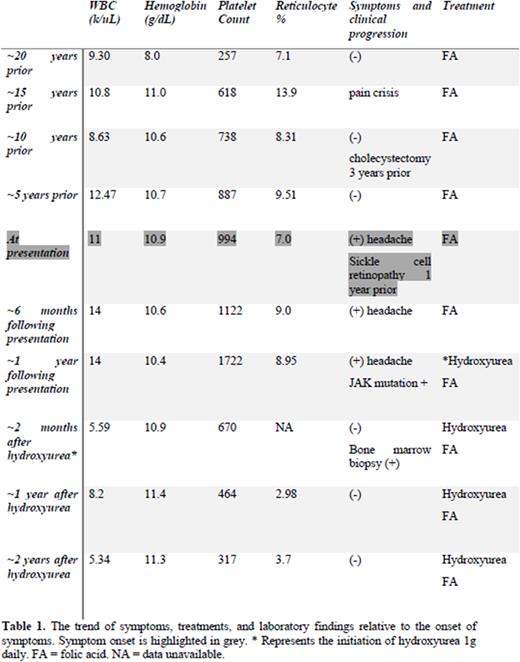
Case Presentation: Here, we report a case of a 38-year-old male with beta 0 thalassemia (HbSB0) SCD who developed a chronic, and unremitting headache of 2 months. Neurological workup of his headache was unremarkable and headache remained unresponsive to various pain medications used by the patient for sickle cell associated pain crises. Laboratory values on presentation were remarkable for WBC 11 k/uL, HgB 10.9 g/dL, platelets 994 k/uL, MCV 72, reticulocyte count 7.0%. A thorough analysis of vasomotor symptoms and laboratory values, when trended over 20 years (table 1), demonstrated that headaches were likely secondary to hyperviscosity, as noted by platelet uptrend and inappropriate hemoglobin elevation for his SCD genotype; in which the expected hemoglobin level is between 6-8g/dL. Laboratory studies demonstrated a JAK2 mutation in peripheral blood with no BCR-ABL mutation detected, excluding chronic myeloid leukemia (CML). Subsequent bone marrow biopsy demonstrated hypercellular marrow (90-95%) with marked erythropoiesis and relatively mild increased granulocytic and megakaryocytic hematopoiesis and mild increase in reticulin fibers, without dysmyelopoiesis; thus excluding myelodysplastic syndrome (MDS). Mutation analysis confirmed JAK2 Val617Phe mutation. Concurrent flow cytometry analysis showed no evidence for leukemia or lymphoproliferative disorder. Together with biopsy data, laboratory data and clinical presentation, the patient was diagnosed with polycythemia vera and essential thrombocytosis. The patient was subsequently managed with Hydroxyurea, with resolution of symptoms presumably due to improvement in blood viscosity due to lowering of platelet levels to 464k/uL.
Discussion: Our report highlights a unique association between MPN in a patient with SCD, diagnostic challenges, and its multifaceted treatment. Our patient presented with unremitting headaches, which can be secondary to either SCD or MPN alone. In patients with SCD severe headache can be associated with ischemic stroke due to vaso-occlusion, hemorrhage, venous sinus thrombosis, aneurysms, meningitis, medication withdrawal or tolerance, bony infarcts, and osteomyelitis. The wide differential diagnosis of headaches in SCD complicates the finding of MPN amongst these patients, and without frequent laboratory monitoring, concomitant vasomotor symptoms would likely remain unnoticed in the patient. Furthermore, our report describes the first documented association of a JAK2 Val617Phe mutation in a patient with SCD. Our case also outlines the use of hydroxyurea as a double edged sword. Interestingly in our patient, hydroxyurea initiation acted as a dual therapy for the management of SCD, through reducing pain crisis episodes, and MPN via platelet count reduction, thereby preventing symptoms of hyperviscosity. Overall, this case highlights a distinctive example of PV and ET in a patient with SCD and its diagnostic challenges, and the first case in the literature to describe JAK2 Val617Phe mutation. Further, our case emphasizes the need to consider vasomotor symptoms and perform a critical analysis of laboratory trends in SCD patients. Future studies may consider a multi-institution retrospective analysis of thrombocytosis in SCD patients to determine if MPN is underdiagnosed in SCD patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal