Abstract
Background: Improvements in medical care for Sickle Cell Disease (SCD) patients in the USA has led to increased survival rates, however, management of comorbidities associated with end organ damage remains challenging. ASH 2019 guidelines do not recommend obtaining screening echocardiogram in asymptomatic SCD patients but suggest management of confirmed Pulmonary Arterial Hypertension (PAH) with specific therapies. For those with Chronic Kidney Disease (CKD) or End Stage Renal Disease (ESRD) requiring dialysis, it is recommended to treat with combination of hydroxyurea and erythropoiesis-stimulating agents as well as consider early referral to transplant nephrology. Our study was aimed to assess the correlation between various characteristics, underlying comorbidities with cardio-pulmonary and renal dysfunction as well as overall outcomes in SCD patients treated at the Henry Ford Hospital sickle cell clinic.
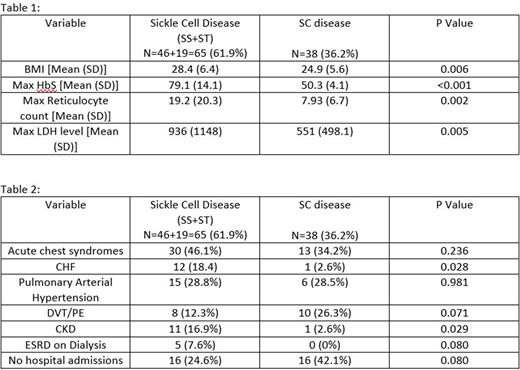
Methods: A retrospective chart review of 105 patients between June 2013-June 2022 was performed. Baseline characteristics including gender, ethnicity, BMI, presence or absence of various comorbidities such as acute chest syndrome, Congestive Heart Failure (CHF), PAH, Deep Vein Thrombosis (DVT)/Pulmonary Embolism (PE), CKD, ESRD requiring dialysis, use of medications such as folic acid, hydroxyurea and newer therapies including voxelotor, crizanlizumab and L-glutamine were obtained. Frequency of ER visits, hospitalizations and blood transfusion requirements were noted. Patients were divided in 2 groups- SS Disease including Sickle/Thalassemia (ST) and SC disease. Continuous variables were compared via ANOVA/Kruskal Wallace Test and categorical variables were compared via Chi Squared Test/Fisher's Exact Test.
Results: In our study, 49.5% were females, 95% were African-American. SS/ST disease type was seen in majority (62.8%) followed by SC disease and 2 patients had sickle cell trait. SS/ST patients were noted to have elevated HbS, reticulocyte count and LDH levels as expected compared to SC disease, whereas those with SC disease were noted to have higher BMI levels likely due less complications.
SS/ST patients were more significantly noted to have diagnosis of CHF (p=0.020) as well as CKD (p=0.029). Interestingly, ESRD requiring dialysis was only seen in SS/ST patients.
69.6% of all patients underwent an echocardiogram evaluation and 28.7% of those had a diagnosis of PAH. In our study, 23.8% with PAH were started on newer therapies.
88.5% of all patients were compliant with folic acid treatment and 34.2% were started on hydroxyurea with significantly higher treatment in those with CHF and elevated HbS levels. Overall, 15.9% patients were started on newer therapies and their use was noted to be significantly higher in patients with CKD and ESRD (p=0.011 and p=0.029 respectively).
Hospitalizations were less frequent in patients with SC disease compared to SS/ST although not statistically significant (p=0.80) and frequency of ER visits was not significantly different between both groups. Also, patients were less frequently hospitalized if they received chronic simple transfusions on outpatient basis.
Conclusion: SS disease patients at our institution had increased likelihood of developing CHF as well as CKD. Of note, those with CKD or ESRD were also more likely to be placed on newer therapies. Based on these findings, we have developed a multidisciplinary management care plan alongside nephrology service.
In our study, about a third of total patients did not have an echocardiogram evaluation, however, 28% of those who had an echocardiogram were noted to have PAH. Therefore, we think that use of screening echocardiogram in all SCD patients could help with early diagnosis of PAH and prompt referral to pulmonary medicine team to prevent potential complications.
Use of hydroxyurea was noted to be significantly higher in those with CHF and newer therapies were more frequently used in patients with CKD and ESRD in our patients. These results encourage better utilization of such therapies in SCD patients with other comorbidities as well as those who have frequent hospitalizations to improve outcomes in the future.
SCD related end organ damage is increasing in incidence with improvement in survival rates and poses a challenge which demands a multidisciplinary system-based care approach.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal