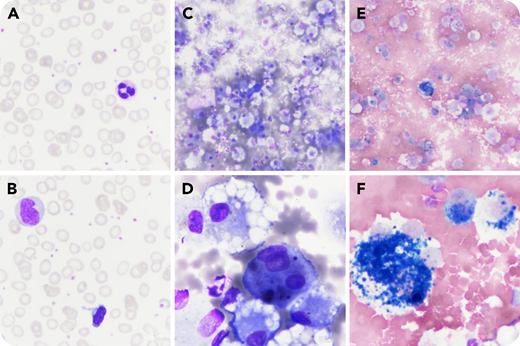
A 14-year-old child presented with nonfebrile dyspnea and hypochromic microcytic anemia without reticulocytosis (hemoglobin, 52 g/L; mean corpuscular volume, 67 fL) with thrombocytosis (524 × 109/L). The blood smear showed dehemoglobinized micro-erythrocytes (microcytic anemia and thrombocytosis) (panels A and B; May-Grünwald-Giemsa stain, magnification x50). Martial deficiency was suspected (serum iron, 3.4 µmol/L; transferrin saturation coefficient, 0.06; C-reactive protein, 13.4 mg/L). Hemoglobin electrophoresis was normal, and the search for glucose-6-phosphate dehydrogenase (G6PD) deficiency was negative. Subsequently, a chest X-ray was performed when respiratory distress with hemoptysis occurred; bilateral and diffuse alveolar infiltrates were observed. An echocardiogram was normal. Cytologic examination of a macroscopically hemorrhagic bronchoalveolar lavage (BAL; panels C-F) revealed the presence of hemosiderin-laden macrophages that suggested a diffuse alveolar hemorrhage (DAH) (panel C: May-Grünwald-Giemsa stain, magnification ×10; panel D: May-Grünwald-Giemsa stain, magnification ×50; panel E: Perls stain, magnification ×10; panel F: Perls stain, magnification ×50). The autoimmune workup was negative. There was no evidence of hypersensitivity to cow’s milk or celiac disease. The diagnosis of idiopathic pulmonary hemosiderosis (IPH) was proposed, and oral prednisone 1 mg/kg once per day allowed improvement of symptoms, correction of anemia, and normalization of the chest radiograph.
In children, the association of iron deficiency anemia, hemoptysis, and bilateral pulmonary infiltrates should raise the possibility of DAH and lead to a BAL. The presence of hemosiderin-laden macrophages demonstrated by Perls stain confirms the diagnosis. The diagnosis of IPH can be made in the absence of infectious, toxic, allergic, autoimmune, or cardiac etiologies.
A 14-year-old child presented with nonfebrile dyspnea and hypochromic microcytic anemia without reticulocytosis (hemoglobin, 52 g/L; mean corpuscular volume, 67 fL) with thrombocytosis (524 × 109/L). The blood smear showed dehemoglobinized micro-erythrocytes (microcytic anemia and thrombocytosis) (panels A and B; May-Grünwald-Giemsa stain, magnification x50). Martial deficiency was suspected (serum iron, 3.4 µmol/L; transferrin saturation coefficient, 0.06; C-reactive protein, 13.4 mg/L). Hemoglobin electrophoresis was normal, and the search for glucose-6-phosphate dehydrogenase (G6PD) deficiency was negative. Subsequently, a chest X-ray was performed when respiratory distress with hemoptysis occurred; bilateral and diffuse alveolar infiltrates were observed. An echocardiogram was normal. Cytologic examination of a macroscopically hemorrhagic bronchoalveolar lavage (BAL; panels C-F) revealed the presence of hemosiderin-laden macrophages that suggested a diffuse alveolar hemorrhage (DAH) (panel C: May-Grünwald-Giemsa stain, magnification ×10; panel D: May-Grünwald-Giemsa stain, magnification ×50; panel E: Perls stain, magnification ×10; panel F: Perls stain, magnification ×50). The autoimmune workup was negative. There was no evidence of hypersensitivity to cow’s milk or celiac disease. The diagnosis of idiopathic pulmonary hemosiderosis (IPH) was proposed, and oral prednisone 1 mg/kg once per day allowed improvement of symptoms, correction of anemia, and normalization of the chest radiograph.
In children, the association of iron deficiency anemia, hemoptysis, and bilateral pulmonary infiltrates should raise the possibility of DAH and lead to a BAL. The presence of hemosiderin-laden macrophages demonstrated by Perls stain confirms the diagnosis. The diagnosis of IPH can be made in the absence of infectious, toxic, allergic, autoimmune, or cardiac etiologies.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal