Abstract
Background:
The use of virtual care rapidly increased during the COVID-19 pandemic to provide adequate care for patients while minimizing contact. Studies in solid tumors show high rates of patient satisfaction with virtual care as well as cost-savings. However, little is known about the application of virtual care in malignant hematology, which includes a heterogenous population of patients often at increased risk of infection. Understanding when virtual care or a hybrid model can be used is crucial for comprehensive patient care.
Methods:
A retrospective review of patients with hematologic malignancies receiving care at Princess Margaret (PM) Cancer Centre in Toronto, Canada from October 2019 to March 2021 was performed. The primary objective was to describe the use of virtual care at three time points: prior to the pandemic, during the initial months of the pandemic, and beyond the initial months. Patients were included in the analysis if they had a clinical visit for their hematologic malignancy. Patients were excluded if they were presenting for treatment-related visits or blood count checks. All methods of virtual care, including phone visits and teleconferencing, were included in the analysis. Patient satisfaction with virtual care was assessed using responses to the Your Voice Matters survey administered from September 2020 to April 2021, a provincial survey of patient-reported experience.
Results:
A total of 93472 visits for 23162 patients were identified at PM from October 2019 to March 2021 (55% of visits for ambulatory clinic appointments). Mean age was 60 years (range 18-103 years) and 45% of patients were female (N = 23162). Ambulatory clinic appointments for new consultation or follow-up care were done in the following clinics: autologous or allogeneic bone marrow transplant (21%, N = 10 747), cellular therapy (0.2%, N = 82), leukemia (26%, N = 13419), lymphoma (32%, N = 16427) and myeloma (21%, N = 10711).
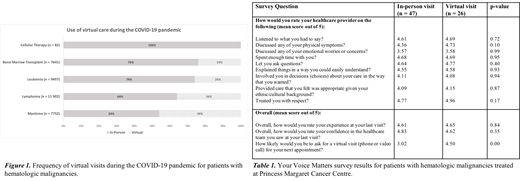
From October 2019 to March 2020, there were 14512 visits, of which nearly 100% were in-person (N = 14511). From March 1 2020 to September 1 2020, there were 19179 total visits, of which 36% were virtual, with the majority of visits by phone (6325 phone visits and 567 video visits). From September 1 2020 to March 1 2021, there was a small decrease in the use of virtual care (p<0.01), but utilization of phone and video visits continued to be used for 30% of patients (N=17695 total visits; 4964 phone visits and 327 video visits). Virtual care was most often used for patients with myeloma (46%) or lymphoma (36%), as shown in Figure 1.
A total of 75 survey responses for patients with hematologic malignancies followed at PM were available. 67 responses (89.3%) were from patients, with the remaining from caregivers. 47 visits (62.7%) were in-person, 26 visits (34.7%) were virtual, and 2 visits (2.7%) did not have the visit type available. Survey results are shown in Table 1.Results for in-person and virtual visits were very similar, with both groups reporting that their provider listened to their concerns and involved them in making treatment decisions. There was a trend toward providers discussing physical symptoms more for patients who had virtual visits (mean score of 4.73/5 for virtual visit compared to a mean score of 4.36/5, p=0.10). Data on next visit type preference was available for 25 patients who had a virtual visit and 46 patients who had an in-person visit. For patients who had a virtual visit, 36% preferred a repeat virtual visit with 56% having no preference and only 7.7% preferring an in-person visit. For patients who had an in-person visit, 33% preferred their next visit to be virtual, with only 24% preferring their next visit to be in-person and the remaining 43% having no preference.
Conclusion:
The use of virtual care increased substantially during the COVID-19 pandemic and persisted into 2021 with high rates of patient and provider satisfaction. The highest uptake of virtual care was for patients with myeloma or lymphoma. There were no significant differences in patient satisfaction scores for virtual visits compared to in-person visits, and one third of patients preferred a virtual visit after an in-person visit. These findings suggest that virtual care is a feasible and preferred tool for delivering care to a substantial proportion of patients with hematologic malignancies. Further work is needed to determine how to optimally integrate virtual care for specific patient populations.
Prica: Astra-Zeneca: Honoraria; Kite Gilead: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal