Abstract
Background: MRD status is an established predictive marker for progression-free survival (PFS) in CLL following chemoimmunotherapy as well as for fixed-duration treatment with venetoclax and an anti-CD20 antibody. To date, this relationship has not been explored for the combination of Ibr+Ven, an all-oral, once-daily, fixed-duration treatment with complementary mechanisms of action that work synergistically to eliminate CLL subpopulations in distinct tumor compartments. In the primary analysis of the phase 3 international GLOW trial, independent review committee (IRC)-assessed PFS for Ibr+Ven was superior to Clb+O (hazard ratio, 0.216; p < 0.0001). Herein we further investigate MRD outcomes at the time of the GLOW primary analysis.
Methods: GLOW (NCT03462719) enrolled patients (pts) aged ≥65 years or 18-64 years with cumulative illness rating scale score >6 or creatinine clearance <70 mL/min. Pts with del(17p) or known TP53 mutations were excluded. Pts were randomized 1:1, stratified by IGHV mutational and del(11q) status, to Ibr+Ven (3 cycles of ibrutinib lead-in, followed by 12 cycles of Ibr+Ven) or 6 cycles of Clb+O. The primary end point was PFS assessed by IRC and rate of undetectable MRD (uMRD; <10 -4) was a secondary end point; additional MRD analyses reported here are exploratory. MRD samples were collected for responders every 3-4 months in peripheral blood (PB) and at Months 9 and 18 in bone marrow (BM). MRD was evaluated using next-generation sequencing (NGS; clonoSEQ) and 8-color flow cytometry. PB/BM concordance was calculated for pts with uMRD in PB at end of treatment plus 3 months (EOT+3) who had a paired BM sample. Analysis of PFS by MRD status includes pts with known MRD status at EOT+3 and no prior progression, death, or withdrawal.
Results: 106 pts were randomized to Ibr+Ven and 105 to Clb+O. Median age was 71.0 years, 51.7% had confirmed unmutated (u)IGHV, 18.0% had del(11q), and 4.3% had a TP53 mutation. Median follow-up was 27.7 (range, 1.7-33.8) months. MRD results are all via NGS and reported for EOT+3 unless otherwise noted.
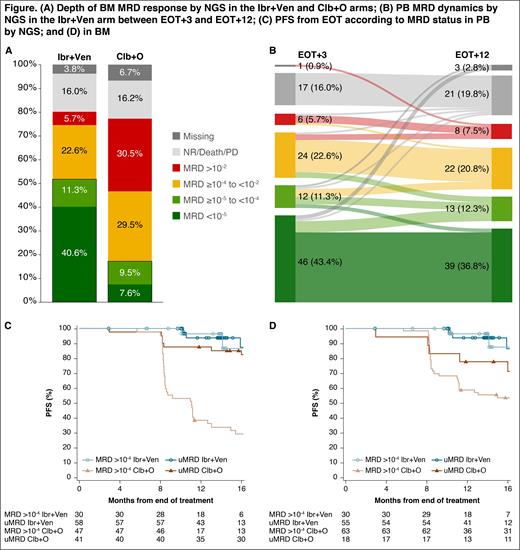
MRD Results at 10 -4: Rate of uMRD was significantly higher for Ibr+Ven vs Clb+O in BM (51.9% vs 17.1%; p < 0.0001) (Fig A) and in PB (54.7% vs 39.0%; p = 0.0259). PB/BM uMRD concordance with Ibr+Ven was 92.9%. In the Ibr+Ven arm, 65.9% (27/41) of pts with a complete response (CR) or CR with incomplete marrow recovery (CRi) and 54.9% (28/51) with a partial response achieved uMRD in BM; rates for Clb+O were 33.3% (4/12) and 16.9% (13/77), respectively. BM uMRD rates were higher for Ibr+Ven vs Clb+O across prespecified subgroups, including bulky disease (≥5 cm), del(11q), and uIGHV . In the Ibr+Ven arm, BM uMRD was higher for uIGHV (58.2%) vs mutated IGHV (44.4%). With Ibr+Ven, 84.5% (49/58) of pts maintained PB uMRD from EOT+3 to EOT+12 vs 29.3% (12/41) with Clb+O. For pts with detectable MRD after Ibr+Ven (n = 30), MRD levels remained stable for most patients from EOT+3 to EOT+12 (Fig B).
MRD Results at 10 -5: Rate of uMRD <10 -5 was higher for Ibr+Ven vs Clb+O in BM (40.6% vs 7.6%) (Fig A), including pts with uIGHV (45.5% vs 5.6%). With Ibr+Ven, PB/BM uMRD concordance at <10 -5 was 90.9% (40/44). Among pts with uMRD <10 -4 in the Ibr+Ven arm, the majority achieved <10 -5 in PB (79.3%) and BM (78.2%), including pts with uIGHV. uMRD <10 -5 in PB was largely sustained from EOT+3 to EOT+12 with Ibr+Ven (80.4% [37/46] of pts) but not Clb+O (26.3% [5/19] of pts) (Fig B).
PFS by MRD Status at 10-4: In the Ibr+Ven arm, PFS rate during the first 12 months after EOT was >90% for pts with uMRD as well as pts with detectable MRD. In contrast, pts in the Clb+O arm with detectable MRD in PB relapsed more quickly than those with uMRD (Fig C). PFS trends were similar according to MRD status in BM (Fig D). Note that not all pts in the Ibr+Ven arm had 12 months' follow-up post-EOT.
Conclusion: All-oral, once-daily, fixed-duration Ibr+Ven demonstrated superior uMRD responses that were deeper and better sustained post-treatment vs Clb+O in elderly or unfit pts with previously untreated CLL. Most pts with uMRD in the Ibr+Ven arm, including those with uIGHV, achieved clearance below 10 -5, and deeper clearance in PB was mirrored in BM. In the Ibr+Ven arm, clinical relapse was infrequent during the first year off treatment for pts with known MRD status at EOT+3 (whether uMRD or detectable MRD), supported by largely sustained uMRD/MRD levels over the same period. Additional follow-up will be important to confirm these early results.
Munir: Janssen, Abbvie, AstraZeneca, Morphosys, Alexion, Gilead, Novartis: Membership on an entity's Board of Directors or advisory committees; Janssen, Abbvie, AstraZeneca, Alexion, Apellis, Gilead, Novartis: Honoraria. Moreno: Abbvie, Janssen, AstraZeneca, Beigene: Membership on an entity's Board of Directors or advisory committees; Abbvie, Janssen, AstraZeneca: Speakers Bureau; Janssen, Abbvie: Research Funding. Owen: Abbvie, AstraZeneca: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen, Roche, Merck, Gilead, Servier: Honoraria, Membership on an entity's Board of Directors or advisory committees. Follows: Roche, Abbvie, Janssen, Takeda, Janpix: Consultancy. Benjamini: AbbVie: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding. Janssens: Abbvie, Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Trael Grant, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Sanofi: Consultancy; Beigene, AstraZeneca: Consultancy, Speakers Bureau. Levin: Roche, Janssen, Abbvie: Other: Travel Expenses, Ad-Board. Robak: AstraZeneca, Abbvie, Janssen, Octapharma, Gilead,Oncopeptides AB, Pharmacyclics, Pfizer, GlaxoSmithKline, Biogen: Research Funding; Biogen, Abbvie, Octapharma, Janssen: Honoraria, Other: Advisory board; Medical University of Lodz: Current Employment. Simkovic: Janssen-Claig, Gilead, Roche, AstraZeneca, Abbvie: Consultancy, Honoraria, Other: Travel Grants, advisiory boards. Voloshin: Janssen, Abbvie, Sanofi, AstraZeneca, Takeda: Other: Clinical Trials, Non-finanfial support, Speakers Bureau; Novartis, Pfizer, MSD, La ROche: Other: Clinical Trials, Non-finanfial support. Vorobyev: Janssen, Roche, Sanofi, Takeda, Biocad, Abbvie: Other: Advisory Boards, Speakers Bureau; Astellas, Novartis, AstraZeneca: Speakers Bureau. Ysebaert: Abbvie, AstraZeneca, Janssen, Roche: Other: Advisory Board, Research Funding. Qi: Janssen: Current Employment. Steele: Janssen: Current Employment. Schuier: Janssen: Current Employment. Baeten: Janssen: Current Employment. Bennett Caces: Janssen: Current Employment. Niemann: Novo Nordisk Foundation: Research Funding; CSL Behring, Genmab, Takeda, Octapharma: Consultancy; Abbvie, AstraZeneca, Janssen: Consultancy, Research Funding. Kater: Abbvie: Honoraria, Other: Ad Board, Research Funding; Genmab, LAVA: Other: Ad Board, Steering Committee; Janssen, AstraZeneca: Other: Ad Board, steering committee, Research Funding; BMS, Roche/Genentech: Other: Ad Board, , Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal