Abstract
Introduction:
Starting in March 2020, the coronavirus 19 disease (COVID-19) pandemic affected the United States (US) health care system. Many individuals were afraid to seek medical care due to fear of obtaining COVID-19; therefore, there was a high frequency of adults forgoing medical care. Chronic conditions including diabetes, COPD, mental health, and HTN outcomes worsened due to decrease in routine care during the pandemic. Sickle cell disease (SCD) is a chronic blood disorder that causes numerous complications including but not limited to vaso-occlusive crisis, strokes, and chronic kidney disease. Individuals who have routine follow up with a hematologist have been shown to have decreased hospitalizations, ER visits, length of stay, and opiate usage. The Inland Empire region of Southern California is one of the densest hot spots for patient's living with sickle cell disease in terms of disease burden and health care utilization. Therefore, we evaluated how the COVID-19 pandemic affected health care utilizations with individuals with SCD in this area.
Methods:
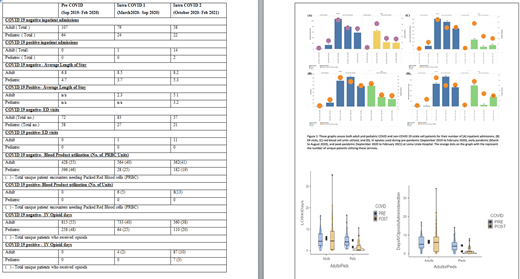
A retrospective analysis of the health care utilization in the inpatient setting was performed at three time points in line with the C.D.C. COVID pandemic declaration (Pre COVID: September 2019 to February 2020, Intra COVID 1: March 2020 to Sept 2020, Intra COVID 2: October 2020 to February 2021). Primary endpoints included emergency room visits, inpatient admissions, and length of stay, blood product utilization, and opioid utilization. Secondary endpoints and analyses included pediatric vs. adult health care utilization disparity and outcomes. Descriptive analysis was done by calculating frequency and percentages for categorical variables and mean and standard deviation for continuous variables.
Results:
Shown in Result TABLE attached .Patients seeking inpatient care for scheduled procedure's/ transfusion were excluded from this analysis. Patients with SCD diagnoses of acute SCD crises (pan crisis /chest syndrome / COVID infection / Pneumonia) were included in assessment. Absolute number of patients per ED visit, patient per Inpatient admission frequency has been shown in more detail in the bar chart in Figure and will be presented in the oral presentation along with detailed data analysis box plots and charts.
Discussion:
Fewer patients' sought timely care for acute SCD event leading to fewer but prolonged hospitalizations, a trend seen in our adult and pediatric patient's across the board during intra COVID 1 and 2 time points, likely due to the fear of contracting COVID infection at an acute health care setting in a declared pandemic . Similarly, we found there were less unique sickle cell patients using the ER for both pediatric and adult patients during the pandemic. There was a decrease in the amount of hospital admission related to sickle cell disease, which was similar to results published in the United Kingdom. More sickle cell vaso-occlusive crisis were being managed at home, likely due to avoidance of COVID exposures at health care facilities, likely thus leading to certain individuals having more severe crisis as shown by increased LOS in our adult population. Additionally, only a few individuals with likely more severe crisis needed more RBC transfusions. The general trend for different patients requiring RBCs and IV opiates decreased during the pandemic. Due to more people foregoing medical care especially in the minority populations who had restrictions to access to healthcare, there was an overall decrease in inpatient healthcare utilization in sickle cell population during the pandemic. Additionally care disparities in outcome of pediatric and adult SCD patients were highlighted by our study. Pediatric patients commonly cared at a center of excellence by the dedicated team of sickle cell stakeholders, seemed to do well overall as compared to adult SCD patients who notoriously have has inequitable access to comprehensive Sickle Cell care globally.
Infrastructure around better outpatient support, care optimization with sickle cell disease modifying agents and timely access to inpatient care even in a pandemic, that is ongoing could be strategies to reduce stress on the health care systems and better utilization of scarce resources in current times of surge from an International health care crisis such as the SAR CoV2 pandemic.
Jain: GBT: Consultancy; CSL Behring: Consultancy, Speakers Bureau; Takeda: Consultancy, Speakers Bureau; Octapharma: Consultancy; Blue Bird Bio: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal