Abstract
A Risk Scoring System for Prognosis of Multiple Myeloma
Background: Multiple myeloma (MM) is the second most frequently-occurring hematologic malignancy characterized by anemia, renal damage, osteolytic lesions and hypercalcemia (Kumar, et al. 2017), without specific prognostic indicators. Protein arginine methyltransferases 3 (PRMT3) is an enzyme which participates in the progression of some malignant diseases (Xiao, et al. 2017). However, the prognostic value of PRMT3 in MM remains unclear. In this study, we developed a risk scoring system based on the expression of PRMT3 to distinguish MM cohorts with different clinical characteristics.
Methods: we integrated 4 datasets from The Cancer Genome Atlas (TCGA) or gene expression omnibus (GEO) and analyzed the correlation between PRMT3 expression and R-ISS stage, diseases progression, clinical characteristics or prognosis. Furthermore, we collected a cohort of newly diagnosed MM and healthy donor samples and then performed qRT-PCR to verify the expression of PRMT3. A risk scoring system was established to point out the prognostic indicator for clinical outcome of MM. The predictive power was evaluated by using Receiver Operating Characteristic (ROC) and Kaplan-Meier survival curve.
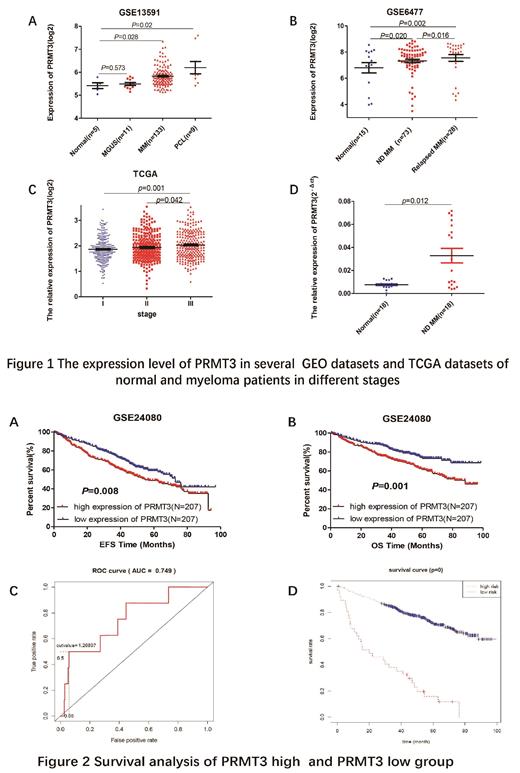
Results: By extensive data analysis, we found the expression of PRMT3 was upregulated during the progression of myeloma (Figure 1 A p=0.573, 0.028, 0.02, respectively). The expression level of PRMT3 in relapsed MM patients was higher than that in newly diagnosed MM patients (Figure 1 B p=0.02, 0.016, 0.002, respectively). Meanwhile, the expression of PRMT3 was also increased in MM patients with advanced R-ISS stage (Figure 1 C p=0.001, 0.042, respectively). Moreover, the validation in a new cohort of MM samples showed the expression of PRMT3 was higher in MM patients compared to normal controls (Figure 1 D p=0.012). MM patients with high expression of PRMT3 showed prolonged Event Free Survival (EFS) and Overall Survival (OS) (Figure 2 A&B EFS: p=0.008, OS: p=0.001). Furthermore, we found the expression of PRMT3 had a positive correlation with B2M(p=0.018), HGB (p=0.001), aspirate plasma cells (p=0.002) and bone marrow biopsy plasma cells (p=0.001 Table not shown). Meanwhile, univariate and multivariate analysis showed that B2M, LDH, ALB, MRI and PRMT3 were independent adverse prognostic factors for OS in MM patients (p<0.001, p<0.001, p=0.0044, 0.0403, 0.0312, Table not shown). Finally, we established a risk scoring system which performed remarkable predicting effectiveness among MM patients. The ROC curve showed that the risk model performed well in 3-year OS (Figure 2 C AUC=0.749). A threshold score 1.26897 was recommended to distinguish the high and low risk score groups. Patients with higher risk score had a shorter OS than those with lower risk score (median 27.45 months vs. 50.13 months, p<0.001 Figure 2 D).
Conclusion: Our study identified that PRMT3 was upregulated in MM patients and that increased PRMT3 was an independent adverse prognostic factor for OS in MM. The risk scoring system based on the expression of PRMT3 provided distinct insights into the prognosis of MM patients.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal