Abstract
Background: Polatuzumab vedotin (Pola), an antibody drug conjugate targeting CD79b received FDA approval in combination with bendamustine and rituximab (Pola-BR) in June 2019. With CAR-T as destination therapy, the option of Pola-BR appears appealing with its superior efficacy and lack of potential interference with CAR-T due to different target antigens. However, clinical concerns remain regarding prolonged lymphopenia associated with benda and CAR-T manufacturing if used before apheresis. We reviewed the single center experience of all patients with exposure to polatuzumab around CAR-T for R/R aggressive NHL treated at Mayo Clinic Rochester.
Methods: A review of patients that received at least one dose of Pola with the intent to proceed to CAR-T between July 1, 2019 and March 31st, 2021 at Mayo Clinic, Rochester were included. Response to therapy was based on 2014 Lugano criteria. Overall survival (OS) was defined as the time from CAR-T infusion to death, and event-free survival (EFS) as the time from CAR-T infusion to disease progression, next treatment, or death. Survival curves were calculated using Kaplan-Meier estimates, and were compared between subgroups using the log-rank test. Cox regression was used for multivariate analysis (MVA).
Results: A total of 22 patients were identified during the study period. Of these 18 (82%), made it to CAR-T infusion (17 axi-cel, and 1 -tisa cel). 3 patients died due to progressive disease (PD) before CAR-T and one achieved complete remission (CR). In the pre-CAR-T Pola cohort (n = 22), the median age was 65.5 years (39-73), 50% were males, 96% had advanced stage and IPI ≥ 3. Median prior lines of treatment were 4.5 (2-6), 73% had primary refractory disease and 50% had myc rearrangement.
19 (86%) patients received Pola as bridging therapy and 8 were exposed to Pola before T-cell apheresis. Bendamustine was included in the treatment for 79% (15/19) for bridging therapy and 63% (5/8) with exposure pre-apheresis. For those in the bridging group, the overall response rate (ORR) was 26% (5/19), with one patient achieving CR with Pola-BR. Disease control (defined as those in a partial response [PR] or stable disease [SD]) was seen in 47% (9/19) patients. One of the 8 patients with pre-apheresis exposure to Pola, required an additional attempt at CAR-T manufacturing after the initial failure.
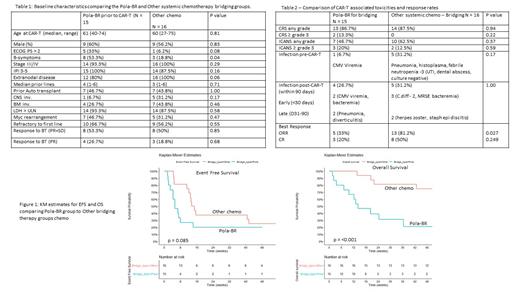
At a median follow up of 48 weeks, the EFS and OS in 18 patient cohort with pre-CAR-T Pola exposure were 6.7 weeks (95% CI, 4.3-not reached [NR]) and 15 weeks (95% CI, 9.7-NR), respectively. At the data cut off (7/25/2021), 78% patients had died. As traditional chemo for bridging is a particularly poor prognostic group, we compared Pola-BR bridging group (n = 15), to other traditional chemo bridge group (n = 16) in our CAR-T database. Both groups had comparable baseline characteristics as shown in Table 1 except for higher proportion of patients with B-symptoms in the Pola-BR group at time of CAR-T. There was also no difference in the inflammatory markers (CRP and ferritin) at LD or peak level after CAR-T. Table 2 shows outcomes between the 2 groups with comparable any grade CRS, neurotoxicity, pre and post CAR-T infection rates. Best response ORR to CAR-T was higher in the other chemo group vs. Pola BR (81.2% vs. 33%, p = 0.027). There was a significant difference in the 6-month OS rate (other 81.3% [95%CI, 54.5-96] vs. pola 33.3% [95%CI, 11.8- 61.6], p = 0.007) but no significant difference in the 6-month EFS rate (other 37.5% [95%CI, 15.2-64.6%] vs. pola 13.3% [95%CI, 1.7-40.5%] p = 0.12) between the 2 groups (figure 1). On univariate analysis within the chemo type bridging cohort (Pola-BR + other traditional chemo, n = 31), presence of B-symptoms (HR 4.72, p = 0.002), ECOG PS > 2 at CAR-T (HR 6.75, p = 0.0008), and type of bridge therapy (pola HR 6.57, p = 0.009) were associated with worse OS whereas a response to bridge (PR+SD, HR 0.39, 0.031) was favorable. On MVA, association was maintained for bridge type (pola, p <0.001) and response to bridge (p <0.001).
Discussion:
Pola based bridge was feasible in this US based cohort without significant issues with CAR-T manufacturing or increased infection rates. However, in this retrospective analysis, use of Pola-BR was associated with inferior outcomes compared to other traditional chemotherapy options. Future studies are required to elucidate whether these difference in outcomes stem from a biological basis versus bias in patient selection.
Wang: TG Therapeutics: Membership on an entity's Board of Directors or advisory committees; MorphoSys: Research Funding; Incyte: Membership on an entity's Board of Directors or advisory committees, Research Funding; Eli Lilly: Membership on an entity's Board of Directors or advisory committees; LOXO Oncology: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding; Genentech: Research Funding; InnoCare: Research Funding. Paludo: Karyopharm: Research Funding. Bennani: Kymera: Other: Advisory Board; Vividion: Other: Advisory Board; Kyowa Kirin: Other: Advisory Board; Daichii Sankyo Inc: Other: Advisory Board; Purdue Pharma: Other: Advisory Board; Verastem: Other: Advisory Board. Ansell: Bristol Myers Squibb, ADC Therapeutics, Seattle Genetics, Regeneron, Affimed, AI Therapeutics, Pfizer, Trillium and Takeda: Research Funding. Lin: Bluebird Bio: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Merck: Research Funding; Kite, a Gilead Company: Consultancy, Research Funding; Novartis: Consultancy; Janssen: Consultancy, Research Funding; Juno: Consultancy; Vineti: Consultancy; Takeda: Research Funding; Gamida Cell: Consultancy; Legend: Consultancy; Sorrento: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal