Abstract
Background: Hematopoietic stem cell transplant (HSCT) using an HLA-identical sibling donor is a well-established cure for sickle cell disease (SCD). Historically, HSCT was only offered to patients with SCD who had suffered severe complications; however, given improved HSCT outcomes, it is now reasonable to consider HSCT for most patients with SCD who have an HLA-identical sibling. Thus, HLA typing of all full siblings of patients with SCD should be a clinical priority to ensure patients are aware of and have access to this therapeutic option.
The primary objectives of this study are to describe the baseline prevalence of HLA typing among a cohort of hospitalized pediatric patients with SCD and to evaluate whether having had HLA typing is associated with certain characteristics. Secondarily, the study describes the acceptability of HLA typing among patients with a healthy (non-SCD) full sibling who had not already had HLA typing at baseline after dedicated outreach to these families.
Methods: Between January 1, 2020 and December 31, 2020 a REDCap database of all hospitalized patients with SCD was prospectively maintained. Patient demographic and clinical information was abstracted via retrospective chart review. To evaluate socioeconomic status, a neighborhood area deprivation index (ADI) was determined for each patient using their home address and the Neighborhood Atlas website (https://www.neighborhoodatlas.medicine.wisc.edu/). ADI is a validated ranking (0-100) of Census Block Groups, considering income, education, employment, and housing quality. A higher ADI represents greater socioeconomic disadvantage.
As part of a clinical outreach initiative, patients' families who had not already had typing at the time of their hospitalization were contacted to determine if the patient has a healthy full sibling and, if applicable, offer sibling HLA typing. This outreach was originally planned to occur in person at the time of hospitalization or clinic follow-up, but due the COVID-19 pandemic it was paused and when resumed conducted mostly via telephone.
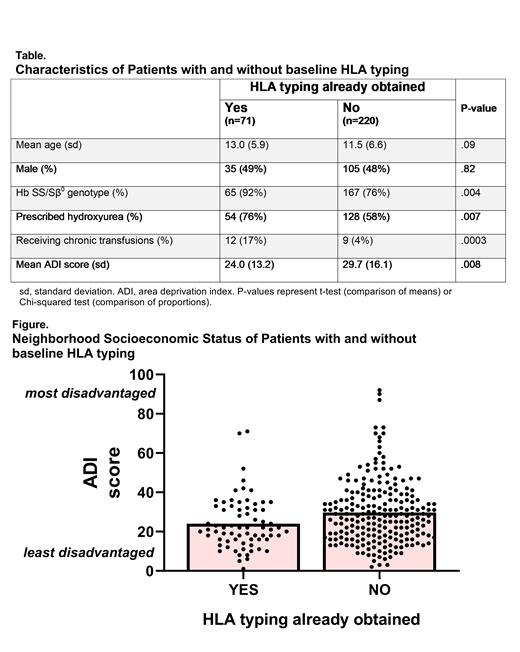
Results: During the 52-week study period, 291 patients with SCD were hospitalized at the study pediatric institution. Seventy-one patients (24%) had already completed HLA typing at the time of their first hospitalization during the study period. These patients with HLA typing at baseline were significantly more likely to have a diagnosis of sickle cell anemia (HbSS/HbSβ 0 genotype) and be on disease-modifying therapy (hydroxyurea or chronic transfusion) compared to patients without typing at baseline (Table). Age and sex were not significantly different between patients with and without typing (Table). The group of patients who did not have HLA typing at baseline had a significantly greater ADI (mean 29.7 vs. 24.0, p=.008) and proportion of patients with a high disadvantage ADI score ≥40 (23% vs. 10%, p=.02), Figure.
Of the 220 patients with no history of HLA typing, the sibling status of 187 patients was determined via outreach to these families as of July 2021. Among these 187 patients, 81 (43%) reported having a healthy full sibling. Among these 81 patients with siblings, after being offered family HLA typing, 42 (52%) were interested and referred for HLA typing, 29 (36%) were undecided, and 10 (12%) declined typing.
Conclusion: Hospitalized pediatric patients with SCD who had already been HLA typed were more likely to have a severe SCD genotype and be on disease-modifying therapy as expected. Patients who had not had HLA typing were more likely to live in a socioeconomically disadvantaged neighborhood. This finding suggests that dedicated outreach to all families regarding HLA typing is needed. Our clinical initiative to offer typing to all hospitalized patients with healthy full siblings was feasible, with a majority of families interested in pursuing HLA typing. Continued work is needed to ensure patients with SCD have equal access to curative therapy regardless of socioeconomic status.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal