Abstract
INTRODUCTION
Cardiopulmonary complications lead to early mortality in adults with sickle cell disease (SCD). We previously showed in a small single-center study that cardiac morphology improves by one year after successful non-myeloablative hematopoietic stem cell transplantation (HSCT). Since cardiac outcomes following HSCT are not well-described, we sought to extend our results to a larger group of SCD patients from the National Institutes of Health (NIH) and University of Illinois Chicago (UIC).
METHODS
The majority of patients received alemtuzumab, 300cGy total body irradiation, and sirolimus; 21 also received pentostatin and cyclophosphamide preconditioning. An echocardiogram (echo) and routine laboratory testing were done at baseline before HSCT and at 1 and 2 year time points. Patients with an echo at least one year following HSCT were included.
A generalized estimating equation regression model approach was used to evaluate echo and laboratory changes from baseline adjusting for age, gender, and site. A more stringent p-value threshold of 0.005 was used for significance given the large number of outcomes tested. The reported p values compare baseline vs 1 year and 1 year vs 2 year changes.
RESULTS
The study population consisted of 88 patients (69 NIH, 19 UIC) who had stable engraftment and were free of dialysis or chronic transfusion therapy. Mean + SD age of patients was 31.5 ± 10.5 years and 36 (41%) are female. Hemoglobin improved significantly in the first year (baseline 8.9 ± 1.5 g/dl, 1 year 12.9 ± 2.3, p < 0.0001), and continued to improve at 2 years (13.6 ± 2.0, p<0.0001). Laboratory results showed improvements in LDH, total bilirubin, and absolute reticulocyte count within the first year after HSCT (data not shown).
Body surface area (BSA) was noted to increase significantly in the first year after HSCT (baseline 1.8 ± 0.2 m 2, 1 year 1.9 ± 0.2, p = 0.0002) and then stabilized in the second year (1.9 ± 0.3, p=0.9). Diastolic blood pressure was 66 ± 12 mmHg at baseline and closely followed the BSA, increasing in the first year (73 ± 11, p < 0.0001) and then remaining unchanged in the second year (74 ± 11, p=0.36). Systolic blood pressure (baseline 118 ± 15 mmHg) did not change significantly.
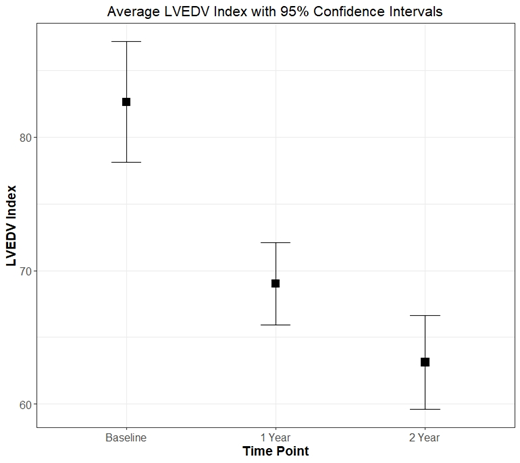
The left ventricular size, as measured by the left ventricular end-diastolic volume index (LVEDVI) was elevated at baseline (82.6 ± 21.5 ml/m2), decreased dramatically at 1 year (69.0 ± 14.7, p < 0.0001), and continued to improve significantly at 2 years (63.1 ± 15.0, p < 0.0001, Figure). LV mass index, which is closely related to volume changes, did not change in the first year (baseline 84.9 ± 23.7 g/m 2, 1 year 85.1 ± 20.9, p= 0.72); however, it improved significantly by 2 years (79.2 ± 17.7, p=0.0003). The left atrial size, as measured by the left atrial volume index, also decreased in the first year (baseline 41.4 ± 12.8 ml/m2, 1 year 28.9 ± 8.7, p < 0.0001) with no change in the second year (27.9 ± 8.2, p=0.05). Diastolic filling parameters, which are independent risk markers of mortality, were seen to parallel the volume changes with baseline E/A ratio decreasing in the first year after HSCT (baseline 1.6 ± 0.6, 1 year 1.4 ± 0.4, p < 0.0001) and then remaining unchanged at 2 years (1.4 ± 0.5, p=0.09).
Tricuspid regurgitation velocity (TRV), which is also a well-known early mortality risk marker in SCD, decreased significantly in the first year (baseline 2.5 ± 0.4 m/s, 1 year 2.4 ± 0.3, p = 0.002), and suggested a trend towards improvement at 2 years (2.3 ± 0.3, p=0.01). In 37 patients with a high-risk TRV ≥2.5 m/s, there was a significant decrease in the first year (baseline 2.9 ± 0.3, 1 year 2.5 ± 0.3, p < 0.0001) and then no change at 2 years (2.4 ± 0.3, p=0.05)
CONCLUSION
Our findings from two independent centers demonstrate significant improvements in cardiac size, mass, diastolic function, and TRV after non-myeloablative HSCT. Volume overload secondary to anemia is responsible for cardiac remodeling in SCD, and as the anemia resolves and high flow rates decrease following HSCT, many of the cardiac changes also reverse. LV volume decreased significantly in the first year, and these improvements, along with decreased LV mass index, continued in the second year. 55% of patients with a high-risk TRV normalized their TRV at 2 years. As diastolic dysfunction and TRV have both been associated with early mortality in adults with SCD, our results suggest that successful HSCT may impact survival. A larger multi-center study with longer follow-up is indicated.
Rondelli: Vertex: Membership on an entity's Board of Directors or advisory committees. Saraf: Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal