Abstract
Background:
Allogeneic hematopoietic cell transplantation (HSCT) is often the optimal and only potentially curative therapy in several high-risk hematologic malignancies. Although human leukocyte antigen (HLA)-matched donors remain the preferred choice for HSCT recipients, haploidentical and umbilical cord blood HSCT has increased access to transplantation. Despite these advances, many patients lack an appropriate donor, in particular the ethnic minorities. The use of mismatched unrelated donors (MMUD) has increased over the years but concerns regarding increased risk of graft versus host disease (GVHD) and non-relapse mortality (NRM) limits the utility of MMUD HSCT. The intensity of the conditioning regimen has a significant impact on survival in case of mismatched donors. We conducted a systematic review and meta-analysis aimed to investigate the outcomes with MMUD HSCT using reduced intensity conditioning (RIC).
Methods:
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines, a comprehensive literature search was performed on three databases (PubMed, Cochrane Library, and ClinicalTrials.gov) from date of inception through February 2021 using the MeSH and entry terms for "hematopoietic stem cell transplantation", OR "hematologic neoplasms", AND unrelated donors" AND "treatment outcome". A total of 2477 records were identified and primary and secondary screening was done. After excluding review, duplicate, and non-relevant articles, we included 6 (4 retrospective, 2 prospective) studies reporting outcomes following RIC MMUD HSCT. The Joanna Briggs Institute (JBI) critical appraisal checklist for studies reporting prevalence data and randomized control trial was used for quality assessment, and all studies were reported as good. Proportions along with a 95% confidence interval (CI) were extracted to compute pooled analysis using the 'meta' package by Schwarzer et al. in the R programming language (version 4.16-2). The variance between the studies was calculated using Der Simonian Laird Estimator.
Results:
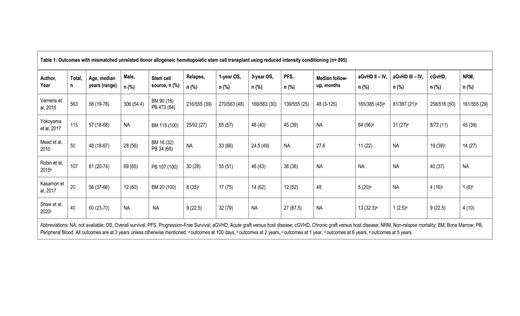
We identified 895 participants in the 6 studies, who had MMUD HSCT with RIC. (Table 1) Median age was 57.5 (18-76) years and 56% (n= 415) were males as reported by four studies (n=740). In five studies with available data (n=855), source of the primary graft was peripheral blood (PB) and bone marrow (BM) in 72% (n=614) and 28% (n=241) of the HSCT recipients respectively. After a median follow-up of 48 (3-125) months, we estimated a pooled overall survival (OS) of 62% (95% CI 0.52-0.72, I 2=84%, n=895) at one year and 43.5% (95% CI 0.33-0.54, I 2 =84% n=855) at three years. The pooled incidence of acute GVHD (grade II-IV), acute GVHD (grade III-IV), and chronic GVHD were 37% (95% CI 0.26-0.49, I 2=81%, n=610), 16% (95% CI 0.07-0.29, I 2=87%, n=542), and 28% (95% CI 0.13-0.47, I 2=95%, n=848) respectively. Progression free survival (PFS) and relapse rates (RR) were 46% (95% CI 0.30-0.62, I 2=92%, n=814) and 31% (95% CI 0.24-0.39, I 2=65%, n=814) respectively. The pooled incidence of non-relapse mortality (NRM) was 23% (95% CI 0.09-0.40, I 2=91%, n=707). Kasamon et al. and Shaw et al. reported 1-year OS of 75-79% with MMUD HSCT using fludarabine, cyclophosphamide and 2 Gy total body irradiation RIC, bone marrow graft and post-transplant cyclophosphamide, sirolimus and mycophenolate for GVHD prophylaxis.
Conclusion:
Mismatched unrelated donor HSCT has shown favorable outcomes with reduced intensity conditioning using a post-transplant cyclophosphamide-based regimen, comparable to the historical outcomes with mismatched related donor (haploidentical) HSCT. MMUD HSCT with RIC can be considered in patients lacking an HLA-matched donor. This strategy will expand access to HSCT in patients with ethnic minorities who often lack a matched donor.
McGuirk: EcoR1 Capital: Consultancy; Allovir: Consultancy, Honoraria, Research Funding; Gamida Cell: Research Funding; Novartis: Research Funding; Kite/ Gilead: Consultancy, Honoraria, Other: travel accommodations, expense, Kite a Gilead company, Research Funding, Speakers Bureau; Astelllas Pharma: Research Funding; Fresenius Biotech: Research Funding; Bellicum Pharmaceuticals: Research Funding; Juno Therapeutics: Consultancy, Honoraria, Research Funding; Novartis: Research Funding; Magenta Therapeutics: Consultancy, Honoraria, Research Funding; Pluristem Therapeutics: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal