Abstract
Introduction: Temozolomide-induced aplastic anemia (TIAA) is a very rare and highly challenging complication of temozolomide (TMZ) chemotherapy. TMZ is a mainstay of therapy in patients with central nervous system (CNS) malignancies. Single-patient case reports and small case series have described variable morbidity and mortality associated with TIAA. However, quantitative evidence describing prognosis, clinical characteristics, and treatment of this entity is absent or very limited.
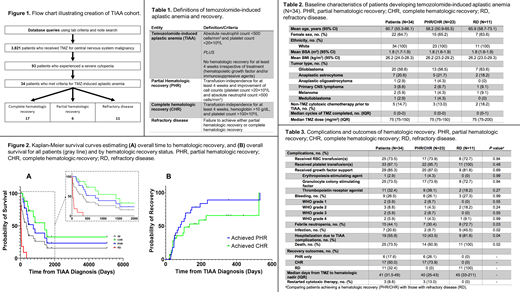
Methods: We performed a 5-center, 22-year observational cohort study of patients with CNS malignancies treated with temozolomide who developed TIAA, retrospectively analyzing prognosis, complications, and recovery. We compared patients who achieved meaningful hematologic recovery [partial hematologic recovery (PHR) or complete hematologic recovery (CHR)] to those who did not recover [refractory disease (RD)]. We used descriptive statistics, T-tests, and chi-square tests to evaluate patient characteristics, outcomes, and laboratory values. Overall time to hematologic recovery and overall survival of patients with PHR, CHR, and RD were estimated using the Kaplan-Meier method and compared using the log-rank test, and a multivariable logistic model evaluated potential predictors of achieving CHR. TIAA was defined using adapted evidence-based severe aplastic anemia criteria incorporating profound cytopenias and a minimum duration (4 weeks) without hematologic recovery (TABLE 1).
Results:
Study Population and TIAA Prevalence. Of 3,821 patients with CNS malignancies receiving TMZ, 34 patients (0.89%) met criteria for TIAA (FIGURE 1). Onset was rapid, with 29 patients (85.3%) developing TIAA before completing a second TMZ cycle (TABLE 2).
Complications and Outcomes of Hematologic Recovery. 23 patients (67.6%) ultimately achieved a hematologic recovery and the remaining 11 patients (32.4%) had refractory disease. Figure 2A illustrates the time from TIAA diagnosis to PHR and CHR for the cohort. In Kaplan-Meier survival analysis, the median time from TIAA diagnosis to PHR was 84 days and the median time to CHR was 134 days. Patients without recovery were more likely to develop serious complications (TABLE 3), including febrile neutropenia (72.7% vs. 30.4%, P=0.03), major infection (45.5% vs. 8.7%, P=0.02), hospitalization (81.8% vs. 43.5%, P=0.04), and death (100.0% vs. 60.9%, P=0.02). This increased risk of complications in patients not achieving hematologic recovery was observed despite a similar median time from TMZ initiation to TIAA diagnosis in the two groups (45 days vs. 40 days). Figure 2B illustrates the overall survival in the entire cohort and by each hematologic recovery subgroup. In Kaplan-Meier survival analysis, median overall survival from the time of TIAA diagnosis was as follows: entire cohort, 355 days; achieved PHR, 752 days; achieved CHR, 1414 days; refractory disease, 28 days (P<0.0001 for comparison of PHR, CHR, and refractory disease). In a multivariable logistic model, none of the evaluated covariates (age, sex, TMZ dose, body surface area, and use of hematopoietic growth factors) were significantly associated with achieving CHR.
Treatment of TIAA and Outcomes of Therapy. 29 patients (85.3%) received hematopoietic growth factors (TABLE 3); no patients were treated with immunosuppression or hematopoietic stem cell transplant. Hematologic recovery rates were numerically higher in patients receiving thrombopoietin receptor agonists vs. those who did not (81.8% vs. 54.2%, P=0.15), but were not higher in patients receiving granulocyte colony stimulating factors vs. those who did not (68.0% vs. 66.7%, P=0.99).
Conclusions: TIAA occurs in less than 1% of patients receiving temozolomide for CNS malignancies, occurring rapidly after TMZ initiation, but is highly morbid and often fatal when it occurs, precluding further use of cytotoxic therapy in the vast majority of patients. In the one-third who do not recover, risks of febrile neutropenia, infection, and hospitalization are increased, and overall survival greatly diminished. Hematologic recovery is potentially aided by the use of thrombopoietin receptor agonists, as has been demonstrated in classical autoimmune aplastic anemia. Further study of TIAA treatment is needed for this serious complication of TMZ therapy.
Forst: Eli Lilly: Current holder of individual stocks in a privately-held company. Al-Samkari: Rigel: Consultancy; Argenx: Consultancy; Moderna: Consultancy; Novartis: Consultancy; Amgen: Research Funding; Dova/Sobi: Consultancy, Research Funding; Agios: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal