Abstract
Background: Acute myeloid leukemia (AML) is an aggressive bone marrow cancer affecting 20,000 adults in the United States yearly. Five-year relative survival remains poor at 29.5%, though this has been steadily increasing. There are no known differences in diagnostic rates between racial and ethnic groups. Previous work has shown being African American is an independent predictor of poorer survival - particularly in impoverished areas and those with Medicaid. We aimed to identify potential racial disparities amongst our AML population - with special attention to insurance coverage, access to care, disease biology, regimen selection, toxicities, referral for allogeneic hematopoietic stem cell transplant (alloHSCT), and overall survival with non-Hispanic Whites as a control.
Methods: This study is a retrospective analysis of patients diagnosed with AML and treated at Virginia Commonwealth University/Massey Cancer Center identified by our data analytics core from June 2018 to December 2020. Data were extracted and manually verified from the electronic medical record into an AML database instrument created in RedCap. Race was determined by self-report. Statistical analysis was performed using GraphPad Prism. Descriptive and inferential statistics were performed with comparisons between groups using an unpaired t-test with Welch's correction or with Fischer's exact test. Overall survival rates were evaluated using Kaplan-Meier analyses and compared using log-rank test. The event date was death and patients were otherwise censored at the date of last contact.
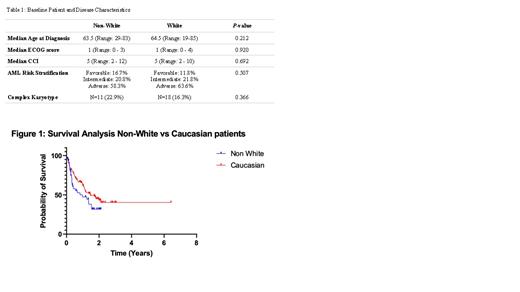
Results: Our cohort consisted of 160 patients: 26.3% African Americans, 68.8% Whites, 1.9% Hispanic/Latinos, 1.9% other or declined to state, and 1.3% were unknown. To analyze the impact of minority populations, Hispanic/Latino and "other" categories were combined with African American into a "Non-White" cohort (N = 48) and compared to the "White" cohort (N = 110). There was no baseline difference in age (p= 0.212), Charleson Comorbidity Index (CCI) at presentation (p = 0.692), or ECOG status (p = 0.920) at presentation (Table 1). Assessment of disease biology, including European Leukemia Network risk stratification (p = 0.507), presence of complex karyotype (p = 0.366) and presence of TP53 mutations (p = 0.776) did not detect a statistically significant difference between the two groups (Table 1). Choice of intensive (vs non-intensive) induction based on physician's discretion was also similar (62.5% in non-White, 68.2% in Caucasians, p = 0.583). Toxicity analysis such as ICU during induction (p = 0.519) and death within 60 days of induction (p = 0.8) showed no difference between groups. In parameters assessing access to care, non-Whites were more likely than Whites to have either Medicaid or no insurance coverage, opposed to private insurance or Medicare (p = 0.0166). Despite this, there was no difference in overall survival assessed by log-rank test (p = 0.068) across all cytogenetic cohorts or with respect to the adverse risk cohort (p = 0.143), though the non-White cohort had a mOS of 286 days (9.4 months) compared to 764 days (25.1 months) in the White cohort. Rates of being lost to follow up were not different between the two groups (p = 0.34). However, rates of alloHSCT were approaching significance with p = 0.0528 favoring Caucasians.
Discussion: Our data suggest similar disease biology at presentation amongst racial and ethnic groups, as well as similar comorbidities, performance status at diagnosis, and choice of induction regimen. As previous research has shown, our minority cohort was more likely to have no insurance or Medicaid than the Caucasian population. However, this did not lead to a statistically significant overall survival difference. Rates of alloHSCT were approaching statistical significance between the groups. This suggests that improving access to transplant might be one of the more effective tools for improving outcomes in this group. Additionally, demographics in the Richmond metro area demonstrate a population of 47% African American and 48% Whites, whereas our data showed 26% African Americans and 69% Whites, with no known strong racial predilection of AML based on SEER data (46% vs 54%, respectively). Thus, concern remains that there may be a significant number of patients with AML who either do not seek care, or present in a condition where treatment is no longer possible.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal