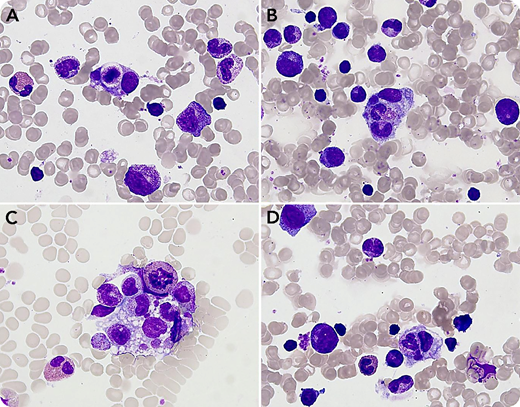
An 11-month-old infant was referred for severe neutropenia of 2-month duration, which was discovered after repeated infections. The blood count showed severe neutropenia (neutrophils 0.1 × 109/L) without anemia or thrombocytopenia. Quantitative immunoglobulin (ie, IgG, IgA, IgM) testing and lymphocyte immunophenotyping results were normal. Examination of the bone marrow revealed a hypercellular marrow that appeared to be reactive with no qualitative abnormality of the marrow cell lines. Granulocytic precursors were increased until the metamyelocyte stage. Strikingly, numerous activated macrophages containing 1 or several neutrophils inside cytoplasmic vacuoles were observed (panels A-D; May-Grünwald-Giemsa stain; 63× objective lens). This selective phagocytosis of neutrophils by marrow macrophages was suggestive of an autoimmune mechanism. Neutrophil-specific autoantibodies against CD16 were detected with an assay for the monoclonal antibody immobilization of granulocyte antigens. A diagnosis of autoimmune neutropenia (AIN) was confirmed.
AIN is a frequent cause of chronic neutropenia in young children. Despite the depth of neutropenia, severe complications are uncommon, and most cases resolve spontaneously (median age of resolution, 2.14 years). Bone marrow aspiration can be omitted in the majority of children, but it may be helpful in symptomatic patients to rule out other diseases. Occasionally, AIN may be associated with intense selective phagocytosis of neutrophils by macrophages in the bone marrow. Phagocytosis of neutrophils only should not be confused with hemophagocytosis (which would suggest a life‐threatening emergency such as hemophagocytic lymphohistiocytosis) because the clinical presentation, morphology, and clinical course of AIN are quite distinct.
An 11-month-old infant was referred for severe neutropenia of 2-month duration, which was discovered after repeated infections. The blood count showed severe neutropenia (neutrophils 0.1 × 109/L) without anemia or thrombocytopenia. Quantitative immunoglobulin (ie, IgG, IgA, IgM) testing and lymphocyte immunophenotyping results were normal. Examination of the bone marrow revealed a hypercellular marrow that appeared to be reactive with no qualitative abnormality of the marrow cell lines. Granulocytic precursors were increased until the metamyelocyte stage. Strikingly, numerous activated macrophages containing 1 or several neutrophils inside cytoplasmic vacuoles were observed (panels A-D; May-Grünwald-Giemsa stain; 63× objective lens). This selective phagocytosis of neutrophils by marrow macrophages was suggestive of an autoimmune mechanism. Neutrophil-specific autoantibodies against CD16 were detected with an assay for the monoclonal antibody immobilization of granulocyte antigens. A diagnosis of autoimmune neutropenia (AIN) was confirmed.
AIN is a frequent cause of chronic neutropenia in young children. Despite the depth of neutropenia, severe complications are uncommon, and most cases resolve spontaneously (median age of resolution, 2.14 years). Bone marrow aspiration can be omitted in the majority of children, but it may be helpful in symptomatic patients to rule out other diseases. Occasionally, AIN may be associated with intense selective phagocytosis of neutrophils by macrophages in the bone marrow. Phagocytosis of neutrophils only should not be confused with hemophagocytosis (which would suggest a life‐threatening emergency such as hemophagocytic lymphohistiocytosis) because the clinical presentation, morphology, and clinical course of AIN are quite distinct.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal