Introduction: Supportive oncology provided by palliative care consultation has proven to prolong survival in randomized studies of patients with advanced cancers, particularly in those with solid tumors. However, the impact of palliative care consultation is less well characterized in patients with hematologic malignancies. We hypothesize that patients with hematologic malignancies are less likely to receive inpatient palliative care consultation. In this study, outcomes of patients with hematologic malignancies who received inpatient palliative care consultation were compared to a control group of disease-matched controls who were not seen by palliative care.
Methods: A retrospective chart review of patients with hematologic malignancies admitted to our inpatient oncology service between 2013-2019 was performed. Data were summarized in SAS v9.4 (SAS, Cary, NC) using descriptive statistics for patients who received palliative care consultation and controls who did not, and these groups were also compared using Wilcoxon rank-sum, chi-square, and Fisher's exact tests as appropriate based on the type and distribution of the data. Multiple logistic regression models with stepwise variable selection methods were used to find predictors of outcomes.
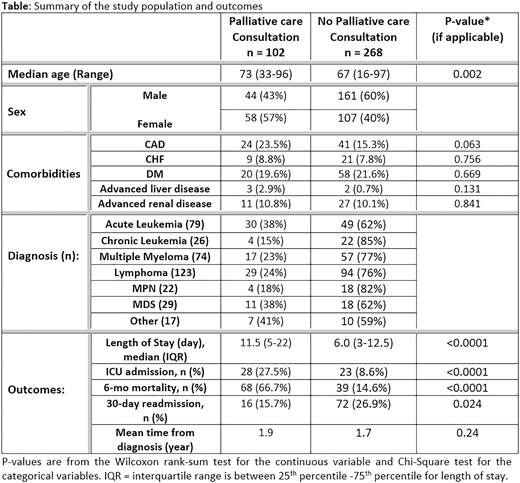
Results: Over the 7-year study period, there were 3,654 admissions to the oncology service, among which 370 hematologic malignancy patients who were actively on treatment were included. Of these, 102 (27%) received palliative care consultation, and the 268 who were not seen by palliative care served as a comparator group. Demographics, disease subgroups, and outcomes are summarized in the table. Groups were similar in terms of comorbidities, as shown in the table. Palliative care consults were greater for patients with acute leukemia and myelodysplasia (38% in each group), and least for those with chronic leukemias (15%) and myeloproliferative diseases (18%). Median length of stay was longer for patients seen by palliative care (11.5 vs. 6 days, P=.001), and these patients were more likely to be admitted to the intensive care (27.5 vs. 8.6%, P<.0001). Readmissions within 30 days of discharge were significantly lower among patients receiving palliative care consultation (15.7 vs 26.9%, P=.024), and 6-month morality was higher (66.7 vs 14.6%, P<.0001). Among all the patients who died within 6-months of admission, 36% did not receive palliative care consultation.
Discussion: Patients with hematologic malignancies who received palliative care consultation had a lower 30-day readmission rate and higher 6-month mortality, despite lack of differences in the time from their cancer diagnosis compared to the control group not seen by palliative care. More than two thirds of all patients did not receive a palliative care consultation, nor did over a third of patients who expired within 6 months of admission. Further research is required to investigate other factors that might warranted palliative care consultation, such as the severity of illness at the time of hospitalization. Results of this study suggest that inpatient palliative care consultation is associated with decreased readmission rate, yet these services are underutilized in patients with hematologic malignancies who are projected to have shorter overall survival.
Braunstein:Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees; Karyopharm: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; Epizyme: Membership on an entity's Board of Directors or advisory committees; Morphosys: Membership on an entity's Board of Directors or advisory committees; Verastem: Membership on an entity's Board of Directors or advisory committees; TG Therapeutics: Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal