CONTEXT: Splicing factor mutations (SRSF2, U2AF1, SF3B1, and ZRSR2) are present in ~50% of myelofibrosis (MF) patients. SRSF2 and U2AF1 Q157 are considered to be high-risk mutations, while the prognostic significance of ZRSR2 and SF3B1 has not been well established. As a group, splicing mutations are associated with cytopenias, the management of which is an area of unmet clinical need in MF.
OBJECTIVE: To describe the clinical characteristics, treatment approaches, and outcomes in MF patients with splicing mutations.
DESIGN: This is a single-institution, retrospective analysis of 133 MF patients with splicing mutations who presented to our institution between 2006 and 2019. PMF, post-ET MF, and post-PV MF were defined according to the World Health Organization and International Working Group criteria, respectively. Baseline variables were compared between patients harboring different splicing factor mutations and different mutations within the same splicing gene. Median overall survival (OS) was measured from time of diagnosis to date of death or censored at last follow up or date of transplant. Kaplan-Meier plots were created to compare LFS and OS among treatment cohorts, and differences were assessed using Log-rank tests.
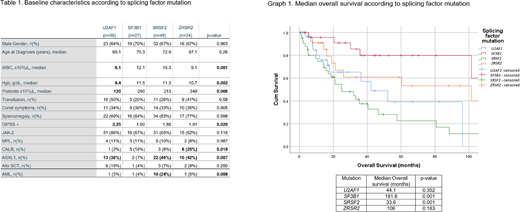
RESULTS: Among 133 MF patients with a splicing mutation, SRSF2 mutations were most common (n = 48), followed by U2AF1 (n = 36), SF3B1 (n = 27) and ZRSR2 mutations (n = 24). Most SRSF2 mutations occurred at P95 (90%). Thirty (83%) U2AF1 mutations occurred at Q157, with 5 (14%) at S34. Fourteen (63%) SF3B1 mutations occurred K666, with 9 (33%) at K700. Thirteen (54%) ZRSR2 mutations were in-frame insertions/deletions, 4 (17%) frameshift mutations, 3 (13%) nonsense mutations and 4 (17%) missense. All frameshift/nonsense ZRSR2 mutations occurred in males. Spliceosome mutations were mutually exclusive but for 2 cases (one had U2AF1 and SRSF2 mutations and the other had SF3B1 and ZRSR2 mutations).
Baseline characteristics were similar between splicing mutations. The presence of a U2AF1 mutation correlated with lower hemoglobin (p 0.018) and U2AF1 Q157 mutations were associated with thrombocytopenia p=0.051) and higher DIPSS-plus scores (p=0.006). Severe thrombocytopenia (platelets < 50 x 109/L) was present in 20 (17%) patients and enriched in those with U2AF1 mutations (n = 9). ASXL1 mutations rarely occurred in conjunction with SF3B1 mutations (p = 0.007).
Among all patients with splicing mutations, median OS was 60.6 months. Median OS was decreased in patients with SRSF2 mutations (33 vs 106 months, p=0.001) compared to those with other splicing mutations. Median OS was increased in patients with SF3B1 mutations compared to patients with other splicing mutations (181 mo vs 42 mo, p = 0.002). Median OS for patients with U2AF1 and ZRSR2 mutations was 44 and 106 months, respectively. Among patients with U2AF1 mutations, the presence of severe thrombocytopenia was associated with inferior survival (13.9 mo vs not reached, p = 0.045). The presence of an SRSF2 mutation was associated with an increased risk of leukemic transformation (24% vs 3%, p = 0.002). Among patients with SRSF2 mutations, median OS in those with documented leukemic transformation was 32.9 mo compared to 48.7 mo in those without (p = 0.17).
CONCLUSIONS: Splicing mutations in MF have unique phenotypic and prognostic correlations. While SRSF2 mutations appear detrimental, SF3B1 mutations correlate with favorable outcomes. While U2AF1 and SRSF2 mutations are considered high-risk in MF, the impact appears driven by cytopenias in the former and leukemic transformation in the latter. This may hold relevance when considering therapeutic approaches in these patients.
Talati:AbbVie: Honoraria; Jazz: Speakers Bureau; Astellas: Speakers Bureau; BMS: Honoraria; Pfizer: Honoraria. Sallman:Celgene, Jazz Pharma: Research Funding; Agios, Bristol Myers Squibb, Celyad Oncology, Incyte, Intellia Therapeutics, Kite Pharma, Novartis, Syndax: Consultancy. Sweet:Takeda: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Incyte: Research Funding; Stemline: Honoraria; Agios: Membership on an entity's Board of Directors or advisory committees; Astellas: Honoraria. Padron:Incyte: Research Funding; Kura: Research Funding; BMS: Research Funding; Novartis: Honoraria. Lancet:Abbvie: Consultancy; Agios Pharmaceuticals: Consultancy, Honoraria; Astellas Pharma: Consultancy; Celgene: Consultancy, Research Funding; Daiichi Sankyo: Consultancy; ElevateBio Management: Consultancy; Jazz Pharmaceuticals: Consultancy; Pfizer: Consultancy. Komrokji:Geron: Honoraria; Novartis: Honoraria; Acceleron: Honoraria; Incyte: Honoraria; Abbvie: Honoraria; Agios: Speakers Bureau; BMS: Honoraria, Speakers Bureau; Jazz: Honoraria, Speakers Bureau. Kuykendall:Blueprint Medicines: Research Funding; BMS: Research Funding; Incyte: Research Funding; Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal