Introduction: Racial and ethnic disparities have been described for patients with aggressive non-Hodgkin lymphomas (NHLs), but few studies have investigated racial disparities in patients with indolent NHLs. Indolent NHLs are a large group of lymphoid neoplasms that include follicular lymphoma (FL), marginal zone lymphoma (MZL), mantle cell lymphoma (MCL), and Waldenstrom macroglobulinemia (WM). Differences in biologic factors (e.g., metabolism of drugs), health disparities (e.g., enrollment in clinical trials), individual factors (e.g., comorbid conditions), and structural barriers (e.g., access to novel therapies) may lead to racial and ethnic disparities in these patients. We aimed to determine whether racial and ethnic disparities exist in the survival of patients with indolent NHLs in the United States.
Method: We used the population-based Surveillance, Epidemiology, and End Results (SEER)-18 database. We included adult patients with FL, MZL, MCL, and WM diagnosed between 2000-2017 who were 18-84 years old at the time of diagnosis. We excluded patients with a history of prior malignancies, missing survival times, central nervous system involvement, and unknown race/ethnicity. Race/ethnicity were categorized as Non-Hispanic White (NHW), Non-Hispanic Black (NHB), Hispanic, Asian/Pacific Islander, and American Indian/Alaska Native. Marginal relative survival (RS) was estimated using the Pohar-Perme method, which estimates net survival within a relative survival framework. Expected survival was determined by matching patients to individuals in the general population by age, sex, race/ethnicity, and year. RS was modeled using Poisson regression where the effect of follow-up time was included as restricted cubic spline with 5 knots. The primary exposure variable in our model was race/ethnicity. Interactions between the main effect and significant covariates were examined (in particular disease histology). All tests of differences were performed at a two-sided alpha of 0.05.
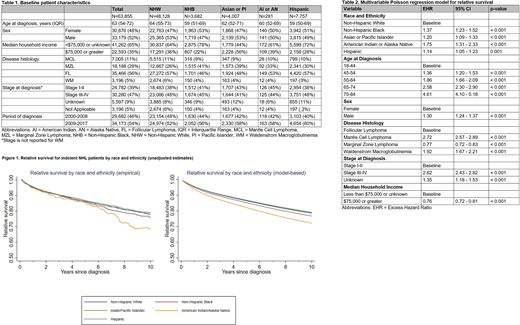
Results: There were a total of 63,855 patients included in our study. Among these patients, 35,466 had FL, 18,188 had MZL, 7,005 had MCL, and 3,196 had WM. Table 1 shows the baseline characteristics stratified based on the race/ethnicity. The median age for all patients was 63 years (IQR = 54-72 years). The majority of patients were NHW (75%). Median length of follow-up was 5.4 years (IQR = 2.2-9.7 years). As shown in Figure 1, RS (unadjusted) for patients with indolent NHL varied according to race and ethnicity. American Indians/Alaska Natives had the lowest survival at 10 years. Estimated 10-year RS (95% CI) was 78% (77-79%) for NHW, 76% (73-79%) for NHB, 79% (77-81%) for Hispanics, 79% (76-81%) for Asians/Pacific Islanders, and 69% (59-76%) for American Indians/Alaska Natives. On multivariable Poisson regression after adjusting for differences in age, sex, stage, median household income, and disease histology, racial/ethnic minorities had significantly increased hazard for excess mortality (NHB=1.37, Hispanic=1.14, Asians/Pacific Islanders=1.20, American Indians/Alaska Natives=1.75) compared to NHW patients (Table 2). There was no significant interaction between race and disease histology (likelihood ratio test p=0.21).
Conclusion: In this large population-based analysis of patients with indolent NHL in the US, we found that racial and ethnic minorities had inferior survival over the past two decades after adjusting for other confounding variables. American Indians and Alaska Natives had the highest mortality followed by NHB, Asians/Pacific Islanders, and Hispanics. One of the plausible explanations for this trend could be related to decreased access to healthcare. Our study emphasizes the need for additional research into racial/ethnic disparities for lymphoma patients.
Epperla:Verastem Oncology: Speakers Bureau; Pharmacyclics: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal