Introduction
Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL) is a unique and clinically distinct subtype of Hodgkin lymphoma (HL), comprising approximately 5% of all HL cases with an annual incidence of about 1-2 cases per million. Compared with classical HL (cHL), NLPHL is more likely to present with limited stage and a more indolent clinical course. Despite these favorable traits, systemic chemoimmunotherapies and/or radiation are often used for initial treatment. Deaths directly from NLPHL are uncommon, with mortality in these patients often attributable to treatment-related toxicities or transformation to aggressive non-Hodgkin B-cell lymphomas.
There is emerging evidence that NLPHL can be treated more conservatively. Active Surveillance (AS), a strategy by which initial treatment is deferred in favor of close observation, has been evaluated in single-institution retrospective studies spanning decades. Borchmannet alreported comparable overall survival (OS) for patients managed with AS versus upfront treatment (Blood, 2019). While encouraging, additional contemporary data are needed to determine if AS is a safe option for NLPHL patients, given advances in supportive care, addition of anti-CD20 therapies, improved radiation delivery, and better diagnostic methods. This retrospective National Cancer Database (NCDB) study evaluates the effect of initial treatment modality on overall survival in a contemporary population of patients with NLPHL to determine if initial AS has comparable OS when compared with initial treatment.
Methods
The National Cancer Database (NCDB) is a nationwide oncology outcomes database for more than 1500 accredited cancer programs in the United States. The NCDB was queried for all patients with the diagnosis of NLPHL, defined by histology code 9659. Filters for inclusion included year of diagnosis from 2010 to 2015, B-cell/pre-B/B-precursor histologic subtype, known treatment status, and with survival data available. Demographic, socioeconomic, treatment modality, and clinical factors such as stage and Charlson-Deyo comorbidity indices were summarized. Chi-square tests were used to correlate factors with treatment status. Kaplan-Meier methods were used to estimate overall survival, and log rank test was used to compare OS between patient groups. Cox proportional hazard model was used to associate patient characteristics with OS, and backwards elimination was used to identify the final Cox model, starting from all factors in univariate analysis.
Results
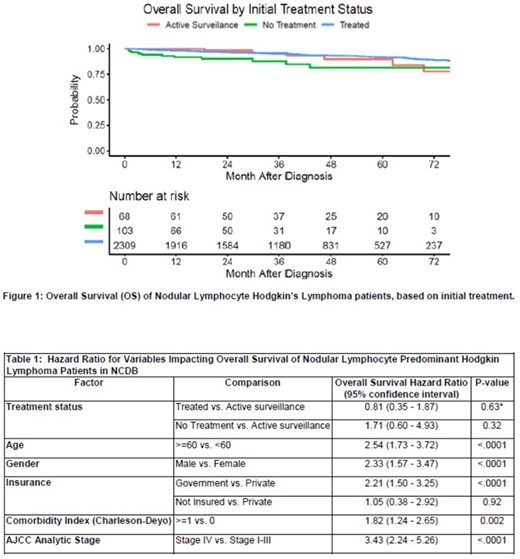
A total of 2,480 patients with NLPHL diagnosed between 2010 and 2015 were included. Of these, 553 patients were older than 60 years (22.3%), 1,616 were male (65%), and 2,110 had a Charlson-Deyo score of 0 (85%) while 370 had a score of ≥1 (15%). 1,627 had Stage I-II disease (65.6%) while 731 had Stage III-IV disease (29.5%). Overall, 2,330 patients were alive (94%) and 150 were deceased (6%), with a median follow-up of 36.8 months (range 0.1 to 94.3 months). Initial management options included: treatment (radiation, chemo/immunotherapy, and/or surgery), no treatment (e.g. palliative care only), or AS. 2,309 patients (93.1%) were initially treated (IT), 103 (4.15%) received no treatment (NT) and 68 patients (2.74%) underwent AS. OS by treatment strategy is shown in Figure 1. In univariate analysis, there was no OS difference between IT vs AS (HR 0.71; 95% CI 0.31-1.61, P=0.41) or NT vs. AS (HR 2.03; 95% CI 0.75-5.51; P= 0.16), but there was a significant difference between NT and IT (HR 2.87; 95% CI 1.56-5.32, P=0.0008). In the final Cox multivariate analysis, there was no significant difference between three treatment groups (overall P=0.10).
Age >60, male gender, those with government insurance, Charlson-Deyo score ≥1, and Stage IV were all associated with decreased OS (Table 1).
Conclusion
In this large NCDB outcomes analysis of 2,480 NLPHL patients, those selected for AS had no difference in overall survival compared to patients who were initially treated. This lends support to emerging evidence that AS is a viable option for a subset newly diagnosed NLPHL patients, as is routine for indolent non-Hodgkin Lymphoma. Future study is needed to identify clinical features associated with a more indolent NLPHL phenotype that may be amendable to less intense initial management.
Hill:Karyopharm:Consultancy, Honoraria, Research Funding;Takeda:Research Funding;Celgene:Consultancy, Honoraria, Research Funding;BMS:Consultancy, Honoraria, Research Funding;Novartis:Consultancy, Honoraria;Kite, a Gilead Company:Consultancy, Honoraria, Research Funding;AstraZenica:Consultancy, Honoraria, Research Funding;Beigene:Consultancy, Honoraria, Research Funding;Pharmacyclics:Consultancy, Honoraria, Research Funding;Abbvie:Consultancy, Honoraria, Research Funding;Genentech:Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal