INTRODUCTION:
Transfusion of red blood cells (RBCs) is a balance between providing benefits for patients while avoiding risks of transfusion. Meta-analyses of randomized controlled trials (RCT) comparing restricted versus liberal blood transfusion showed that there was no significant difference in terms of morbidity, mortality, or risk of myocardial infarction. In fact, the restrictive strategy had a significantly lower risk of all-cause mortality in patients with gastrointestinal bleeding. It also resulted in a significantly lower number of transfused units and a lower number of patients needing a transfusion.
Examining the extent of adherence to the American Association of Blood Banks (AABB) transfusion guidelines in our VA medical center showed that the average transfused units were 1.4 units per person. The Average pre-transfusion hemoglobin (Hgb) was 7.6. 54% received 2 units, whereas 46% received 1 unit.
AIM OF THE WORK:
To improve the blood transfusion practice in our VA medical center to better comply with the (AABB) transfusion guidelines and to establish a culture of change to improve patient safety, minimize risks of transfusion reaction and reduce the cost.
METHODOLOGY:
This is a prospective analysis of transfused patients in the period of November 2019 to April 2020 (n=228) as a continuation of the prior retrospective analysis of randomly selected patients in 2018 (n=162). The data was retrieved from an electronic medical record database, which included patient gender, age, co-morbidities, mean baseline Hgb, pre- and post-transfusion Hgb, hemodynamic status, ordering division, and the number of units transfused.
INTERVENTIONS
We implemented a two-tier auditing system, based on a low and high priority, which reflects the timeline to address non-compliant transfusion orders. Low priority orders were evaluated during the periodic meeting of the transfusion committee, and high priority orders were addressed within a few hours of the transfusion order. All transfusion orders of Hgb > 7-8 g/dL were flagged with low priority, whereas those with Hgb > 8 g/dL and/or with orders exceeding one unit were flagged with high priority. The appropriate approval was obtained through the institutional review board (IRB), patients' consents for enrollment, and anonymity was maintained all through the study.
RESULTS:
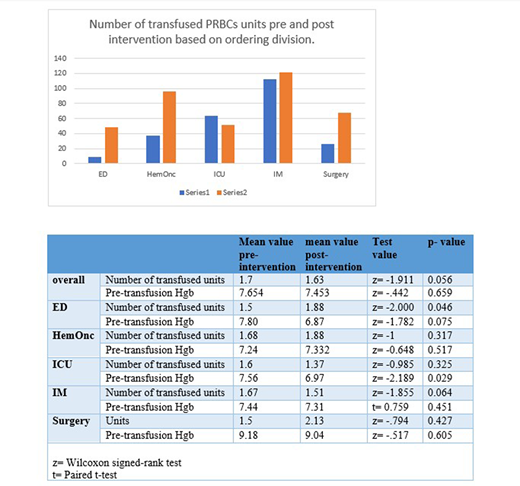
The total number of transfused PRBC units was 386 units with a mean of 1.6 units per patient compared to 1.7 units in the pre-intervention group (p=0.056).
The average Hgb before transfusion was 7.7 mg/dL compared to 7.5 mg/dL in the pre- versus the post-intervention group (p=0.659). Comparing the pre-transfusion Hgb values in both groups per ordering division showed that the average Hgb values were lower after the intervention among all divisions except for the hematology/oncology department. This difference was statistically significant in the Intensive Care Unit (ICU). In terms of the number of transfused units, overall, there was a decrease in the number of transfused units, however, this was not statistically significant.(table 1) The department with the highest number of transfused units was internal medicine.
DISCUSSION:
Our study showed that the application of an auditing system within the electronic medical system resulted in significant improvement in the transfusion practice in the ICU department. The lack of significant effects among other departments can be attributed to the lower number of cases in the pre- versus post-intervention cohorts, e.g. 22 versus 50 in the Hematology/Oncology department and 6 versus 26 in the Emergency Department. Besides, it was difficult to gauge the reasoning for blood transfusion among the different departments whether it was for objectively significant blood loss despite the stable hemodynamics, or due to symptomatic anemia.
The overall acceptance of the new system should be further investigated through a qualitative study e.g. individual interviewing or group discussions to explore reasons for possible resistance to change.
CONCLUSION:
Changing the transfusion order can help in improving the transfusion practice in healthcare facilities. However, this strategy alone may not be effective, and further investigations into the root causes of the non-significant change in some departments are needed. Enforcing the electronic auditing system along with staff development workshops may result in better outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal