Introduction: Life expectancy for long-term survivors of allogeneic hematopoietic stem cell transplant (allo-HCT) is significantly lower compared to that of the age-matched general population, despite a relatively low primary disease relapse rate >2 years post-transplant. Long-term transplant-related complications instead account for most mortality in this patient population. These include chronic graft-versus-host disease (cGVHD), infection, organ failure, and secondary cancers. In addition, gender is emerging as a critical determinant of outcome in the immediate post-transplant setting. However, less is known regarding gender effects on outcomes of long-term survivors. We retrospectively investigated the impact of recipient gender and donor-recipient gender mismatch on outcomes of long-term survivors of allo-HCT.
Methods: We performed a retrospective analysis using Duke University's Adult Blood and Marrow Transplant database, supplemented by individual patient chart review. Inclusion criteria consisted of long-term survivors of first allo-HCT, excluding syngeneic, between 1995 - 2015 for a hematologic malignancy. A long-term survivor is defined as having been alive with documented follow-up to at least five years following allo-HCT. Patient characteristics were summarized as count (%) for categorical variables and median (interquartile range) for continuous variables. Fisher's exact tests or t-tests were used to compare difference between groups. Overall survival was estimated using the Kaplan-Meier method and multivariable Cox proportional hazard model. Patients who had received cord blood allograft were excluded from donor-recipient gender survival analyses. SAS version 9.4 (SAS Institute, Cary, NC) and R 3.5.0 were used to perform statistical analyses.
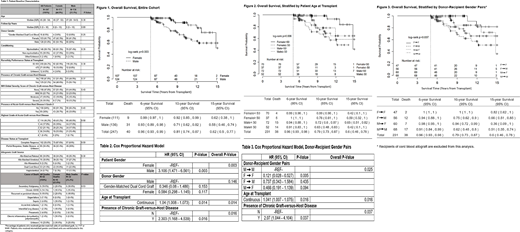
Results: Over this 20-year period, 1103 patients underwent allo-HCT, with 247 (22%) meeting inclusion criteria. Of these 247, males and females had similar demographic and treatment characteristics (Table 1). However, significantly more deaths after the 5-year landmark occurred in male recipients (Figure 1, p value=0.003). To estimate whether this was due to the general population-wide shorter life expectancy for males, we performed Kaplan-Meier estimates of survival for patients aged < 50 years at transplant and aged ≥ 50 years at transplant, with similar results for both groups (Figure 2, p value=0.006). Interestingly, donor gender did not have a significant impact on overall survival in multivariate analysis (Table 2), and differences in overall survival of donor-recipient gender pairs was driven by patient gender (Figure 3, p value =0.007). A separate multivariate analysis of interaction between donor-recipient gender pairs further demonstrated that significant differences in overall survival were due to patient gender (Table 3). In addition to patient gender, only cGVHD retained significance as a covariate with impact on overall survival in multivariate analysis (Table 2, Table 3). Men experienced slightly higher rates and increased severity of cGVHD, and a greater percentage of cGVHD-related mortality as compared to females, though these findings were not statistically significant (Table 1).
Conclusion: In this long-term survival analysis of allo-HCT adult patients, one of the only to include follow-up to 15 years, our results show that women survive significantly longer than men irrespective of their age at transplant. This outcome is independent of other common pre-transplant prognostic indicators such as donor gender or performance status at transplant. Inferior survival for males is consistent with survival outcomes described in another large and fully risk annotated HCT cohort, and in solid organ transplants such as lung and kidney. Gathering evidence suggests a biologic basis for long-term gender-determined outcomes, possibly due to differing rates or severity of cGVHD or sustained alloimmune tolerance in females. Male patients should be counseled on their possible increased long-term risk. Prospective and larger studies are warranted to validate these retrospective clinical results.
Rizzieri:Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jazz: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Seattle Genetics: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Stemline: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Incyte: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Kite: Honoraria, Speakers Bureau; Karyopharm: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; abbvie: Membership on an entity's Board of Directors or advisory committees; AROG: Membership on an entity's Board of Directors or advisory committees; Bayer: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Celltrion: Membership on an entity's Board of Directors or advisory committees; Mustang: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Teva: Membership on an entity's Board of Directors or advisory committees; Acrobiotech: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal