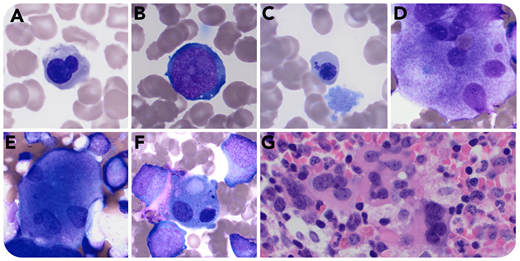
A previously healthy 5-month-old girl was hospitalized for fever (39.6°C) and intermittent tachycardia. Five weeks earlier, her father had tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). She had both SARS-CoV-2 by reverse transcription polymerase chain reaction (nasopharynx) and anti–SARS-CoV-2 immunoglobulin G and was experiencing severe, progressive anemia (6.6 g/dL) and thrombocytopenia (36 × 103/µL) with leukopenia (3.2 × 103/µL). Bone marrow aspirate showed left-shifted granulocytes with reactive changes. A subset (<10%) of erythroblasts demonstrated nuclear lobation (panel A; original magnification ×1000; Jenner-Giemsa stain), irregular nuclear contours and cytoplasmic vacuoles (panel B; original magnification ×1000; Jenner-Giemsa stain), and detached nuclear fragments (panel C; original magnification ×1000; Jenner-Giemsa stain). Few (<10%) megakaryocytes showed separated nuclei (panels D-E; original magnification ×1000; Jenner-Giemsa stain) or micromegakaryocytes (panel F; original magnification ×1000; Jenner-Giemsa stain). Core biopsy was hypercellular, demonstrating increased megakaryocytes with focal clustering (panel G; original magnification ×500; hematoxylin and eosin stain). There was no evidence of hemophagocytic lymphohistiocytosis. Other significant findings included hypoalbuminemia, markedly increased brain natriuretic peptide (3617.5 pg/mL), elevated D-dimer (8.06 µg/mL), and mild to moderate tricuspid valve regurgitation with small pericardial effusion. All symptoms and laboratory findings of multisystem inflammatory syndrome in children (MIS-C) resolved with methylprednisone treatment. The patient remained healthy, with complete recovery of all lineages and no other instances of cytopenia during outpatient follow-up for 6 weeks.
We report an atypical case of MIS-C associated with COVID-19. This case raises the possibility that very young pediatric patients may demonstrate more pronounced hematologic effects, including peripheral cytopenias. Dyserythropoiesis and dysmegakaryopoiesis may reflect marrow stress responses or hint at an underlying germ line predisposition syndrome contributing to this unusual presentation.
A previously healthy 5-month-old girl was hospitalized for fever (39.6°C) and intermittent tachycardia. Five weeks earlier, her father had tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). She had both SARS-CoV-2 by reverse transcription polymerase chain reaction (nasopharynx) and anti–SARS-CoV-2 immunoglobulin G and was experiencing severe, progressive anemia (6.6 g/dL) and thrombocytopenia (36 × 103/µL) with leukopenia (3.2 × 103/µL). Bone marrow aspirate showed left-shifted granulocytes with reactive changes. A subset (<10%) of erythroblasts demonstrated nuclear lobation (panel A; original magnification ×1000; Jenner-Giemsa stain), irregular nuclear contours and cytoplasmic vacuoles (panel B; original magnification ×1000; Jenner-Giemsa stain), and detached nuclear fragments (panel C; original magnification ×1000; Jenner-Giemsa stain). Few (<10%) megakaryocytes showed separated nuclei (panels D-E; original magnification ×1000; Jenner-Giemsa stain) or micromegakaryocytes (panel F; original magnification ×1000; Jenner-Giemsa stain). Core biopsy was hypercellular, demonstrating increased megakaryocytes with focal clustering (panel G; original magnification ×500; hematoxylin and eosin stain). There was no evidence of hemophagocytic lymphohistiocytosis. Other significant findings included hypoalbuminemia, markedly increased brain natriuretic peptide (3617.5 pg/mL), elevated D-dimer (8.06 µg/mL), and mild to moderate tricuspid valve regurgitation with small pericardial effusion. All symptoms and laboratory findings of multisystem inflammatory syndrome in children (MIS-C) resolved with methylprednisone treatment. The patient remained healthy, with complete recovery of all lineages and no other instances of cytopenia during outpatient follow-up for 6 weeks.
We report an atypical case of MIS-C associated with COVID-19. This case raises the possibility that very young pediatric patients may demonstrate more pronounced hematologic effects, including peripheral cytopenias. Dyserythropoiesis and dysmegakaryopoiesis may reflect marrow stress responses or hint at an underlying germ line predisposition syndrome contributing to this unusual presentation.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal