Introduction
Thalassemia is the most prevalent inherited hemoglobinopathy characterized by defective synthesis of β chain, leading to ineffective erythropoiesis. In India, 3.2% (1 in every 25 people) are carriers of beta thalassemia. Management of thalassemia includes transfusion support, adequate iron chelation and prevention of undue extramedullary erythropoiesis. Red blood cell aggregation, aggregate strength and oxygen transport potential of blood are abnormal in both homozygous sickle cell anemia and sickle - hemoglobin C disease. Both clinicians and families of these patients realize that the main challenge is obligation of life long blood transfusion and iron chelation therapy in order to have a normal life. Thalidomide, an immunomodulatory drug, has therapeutic effect in fetal Hemoglobin (HbF) induction but exact mechanism of action is not known yet. Hence, this drug has been tried in thalassemia intermedia (TI) and had shown significant effect in decreasing transfusion requirement.
Primary aim of our study was to evaluate the clinical response of thalidomide and/or Hydroxyurea (HU) in transfusion dependent beta thalassemia (TM and TI). The secondary aim is to study the toxicity profile of this drug in our study population.
Methods
It is a retrospective study which included beta TM and TI patients from August-2015 to November-2018, who received thalidomide with or without hydroxyurea. Dose used was 10-20 mg/kg/day & 25-100 mg/day for HU and thalidomide respectively. Study was approved by Institutional Review Board.
Results
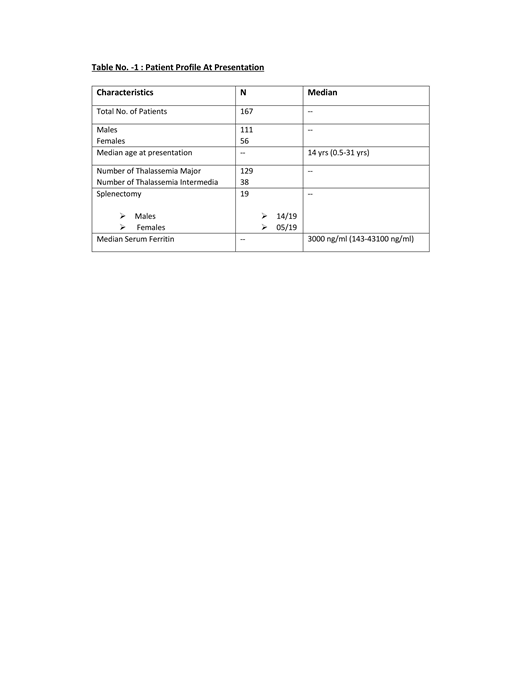
We studied 167 patients (TM=129 and TI=38) with males (n= 111) and median age 14 (0.5-31) years. At presentation, median size of liver and spleen was 4 (1-12) cms and 3 (1-16) cms respectively. Nineteen patients were post splenectomy. Median age at first transfusion was 9 (1-144) months. Median duration between transfusions was 20 (10-180) days. Median packed cell transfusion per year was 18.2 (2-36.5). (Table-1).
Median dose of HU was 500 (250-500) mg & thalidomide was 50 (25-100) mg. Median duration of thalidomide therapy was 9 (1-73) months and HU was 8 (1-183) months. Median Hb post treatment at day 90 for TI was 9.1 gm/dl (6.7-13) gm/dl and TM was 9.1 (6.2-13) gm/dl. Median duration of transfusion free period was 15 months (1-38 months) till last follow-up. Post treatment median size of liver and spleen was 3 (2-11) cms & 2 (1-14) cms respectively. Increased duration between transfusions was observed in 17 patients with median duration of 40 (18-90) days between transfusions.
Most common toxicities observed were constipation=1, neutropenia=9, deranged liver function =6 followed by skin rash=4. Thrombosis, Hepatitis-A and excessive fatigue was seen in 1 patient each.
At last follow-up, 78 (46.7%) patients were transfusion free whereas 37 (22.1%) were transfusion dependent, duration of transfusion increased in 17 (10.2%) patients, 3 (1.2%) patients abandoned treatment and 6 (3.6%) patients to be assessed yet as they didn't complete their 3 months of therapy at last follow-up. No follow-up records available for 26 (15.5%) patients so response could not be assessed.
Conclusion
With the use of minimal doses of thalidomide, transfusion independency and thereby reduction in iron overload can be achieved in patients with transfusion dependent beta thalassemia patients. But one needs to be cautious to monitor the side effects commonly encountered in our study. Large population studies and longer follow ups are required to define the potential use of this immunomodulatory drug in hemoglobinopathies, which can be an effective and affordable treatment option for transplant ineligible patients.
No relevant conflicts of interest to declare.
Thalidomide is an HbF inducer, which by increasing HbF levels, decreases ineffective erythropoiesis and reduces transfusion burden in patients with TDT
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal