
Background: The use of immunosuppressive therapies in the management of non-malignant immune-mediated hematologic disorders (NMIHD) leads to an increased risk of infections. Preventive strategies, such as immunization and infectious disease (ID) screening, reduce the burden of infectious complications. However, lack of compliance to available guidelines among healthcare providers (HCP) represent a major concern. The present study was performed to assess adherence by HCP to national guidelines and recommendations for the prevention of infectious complications in patients (pts) treated for a NMIHD with the goal to identify areas where interventions can be implemented to improve awareness.
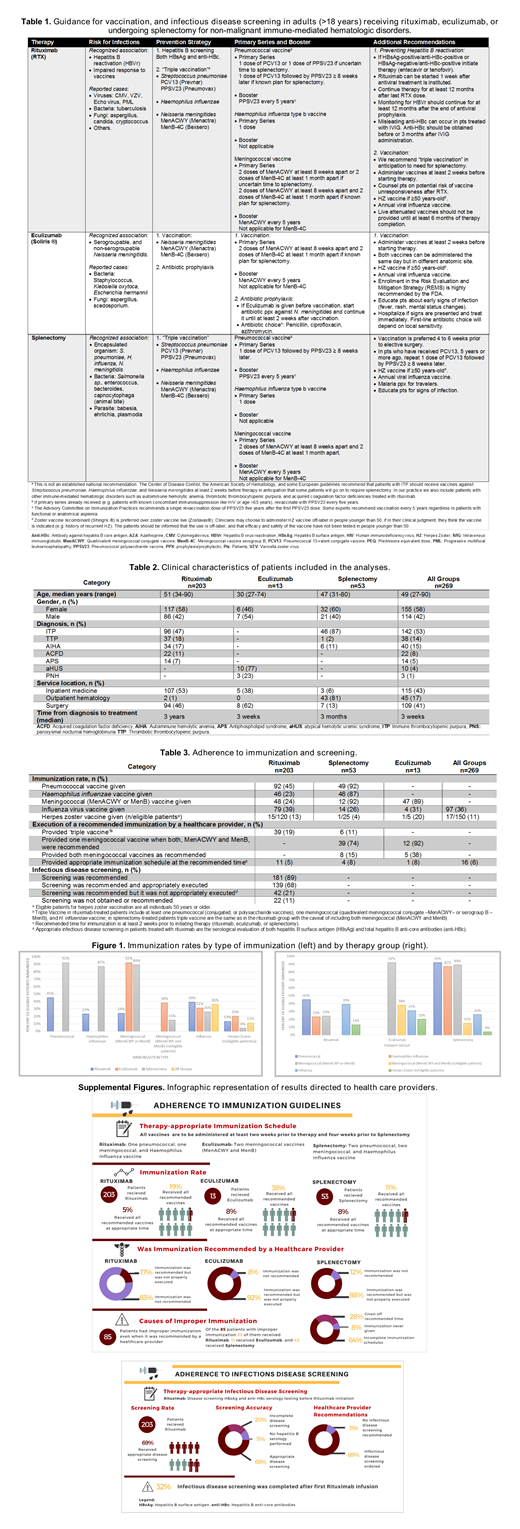
Methods: We retrospectively analyzed pts diagnosed with AIHA, acquired coagulation factor deficiency (ACFD), TTP, ITP, aHUS, PNH, and antiphospholipid syndrome (APS) between January 2016 and July 2018 at an academic medical center (University of North Carolina). Pts had to have received either rituximab (RTX), eculizumab, or splenectomy. Adherence to existing strategies was assessed based on available recommendations from recognized national entities (e.g. CDC, ACIP), and clinical societies (e.g. ASH) (summarized in Table 1). Immunizations considered for analysis included: pneumococcal, meningococcal and Haemophilus influenzae vaccines ('triple vaccine' if received all together). We considered 'adherence to an immunization recommendation' when, depending on the diagnosis and treatment employed, pts received all recommended vaccines at least 2 weeks prior to therapy or 4 weeks if splenectomy. Adherence to ID screening in pts receiving RTX therapy was defined as pts screened for both hepatitis B surface antigen and total core antibodies. Influenza virus and herpes zoster (HZ) immunization rates were also analyzed.
Results: 269 pts from six UNC-affiliated hospitals were included. Pts clinical characteristics are summarized in Table 2. Overall, only 6% of all evaluable pts were appropriately immunized as recommended by national guidelines (5%, 8%, and 8%, for RTX, eculizumab, and splenectomy, respectively) (Table 3). Immunization rates are summarized in Figure 1. In the eculizumab group, although 92% of HCP recommended and prescribed meningococcal immunization, only 38% (n=5/13) received both vaccines (54% either, 8% none). Likewise, although 89% (n=47/53) of pts undergoing splenectomy had received a 'triple vaccine', only 11% of pts received guideline recommended vaccines (both pneumococcal and meningococcal vaccines) and only 8% were appropriately vaccinated by receiving all indicated vaccines at least 4 weeks prior to their scheduled surgery. 68% of pts treated with RTX were appropriately screened for hepatitis B, with lower rates found in young women (screening rate: 77% age >50 vs. 58% ≤50 years, p<0.01; 83% male vs. 58% female, p<0.01) diagnosed with TTP or APS (ITP 74%, AIHA 79%, ACFD 77% vs. TTP 46%, APS 55%, p=0.01). Lastly, 36% of pts received annual influenza virus vaccine, and 11% of eligible pts the HZ vaccine.
Conclusion: To the best of our knowledge, there have been no studies conducted in the U.S. assessing adherence to infectious prevention guidelines among different NMIHD. We found that in pts with NMIHD undergoing immunotherapy or splenectomy, many pts received either incomplete recommended immunizations or the immunization was administered too close in proximity to the immunosuppressive therapy or splenectomy, both resulting in impaired immunologic response to vaccines. In addition, only two thirds of pts receiving RTX had pretreatment screening for hepatitis B infection at odds with national recommendations of 100%. Lastly, low immunization rates against influenza virus and HZ were found. Based on these results, we created infographics (supplemental figure), an "easy-to-use" pocket brochure summarizing recommendations (Table 1), and we are building immunization reminders when electronically prescribing immunotherapy, with the aim of improving HCP awareness in our health care system. Although we are unsure about other institution's compliance rate, we suspect that non-compliance to immunization is a systemic problem across the U.S. We will disseminate this data hoping to replicate this study at other academic institutions. There is an urgent need for the development of strategies to improve HCP awareness and adherence to infectious prevention guidelines!
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal