Background: Frailty is associated with poor tolerance to chemotherapy and mortality. While recent evidence suggests measures of frailty such as gait speed predict survival in older patients with hematologic malignancies such as lymphoma (Liu, Blood, 2019), its predictive ability has not been compared to disease-based prognostic risk scores.
Methods: From February 2015 to April 2019, all patients aged 75 years and older who presented for initial consultation for at the Dana-Farber Cancer Institute for diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL) and Waldenstrom macroglobulinemia (WM) were approached for a screening frailty evaluation by a trained research assistant. As part of the evaluation, 4-meter gait speed was assessed (at normal pace with non-ambulatory patients recorded as having a speed of zero). Disease-specific prognostic scores were obtained retrospectively, including the International Prognostic Index (IPI) for DLBCL, the Follicular Lymphoma International Prognostic Index (FLIPI) for FL, and the International Prognostic Scoring System for Waldenstrom Macroglobulinemia (ISSWM). Univariate and multivariable Cox proportional hazard models were used to determine predictors of overall survival (OS; from date of screening geriatric assessment) including gait speed and disease-specific scores. Those with incomplete risk data excluded from disease-specific analyses. Hazard ratios and generalized R2 (higher the R2, stronger association with OS) were also calculated.
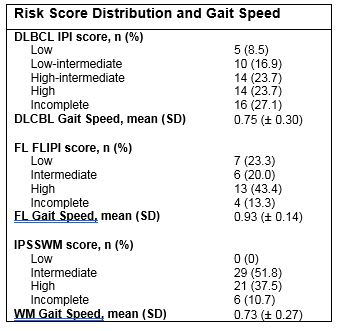
Results: A total of 145 patients were included, 59 with DLBCL, 30 with FL, 56 with WM. Median age was 79 (IQR 77 to 82) and 42.1% were female. For the overall cohort, mean gait speed was 0.78 (±0.27). Risk score distribution and disease-specific gait speed are presented in the table. With a median follow-up of 20.9 months (IQR 10.2 to 34.5), median OS was 14.4 months for DLBCL, 17.2 months for FL and 32.0 months for WM. Disease-specific prognostic scores were not predictive of survival for DLBCL (p = 0.76) or FL (p = 0.22) but were for WM (p = 0.04). Overall, faster gait speed was significantly predictive of OS (HR 0.10, 95% CI 0.03 to 0.32, p < 0.0001) for all three lymphomas combined, which would mean an HR of 0.56 for an increase of 0.25 m/s of gait speed. In disease-specific analyses, faster gait speed was predictive of survival for DLBCL (HR 0.10, 95% CI 0.02 to 0.46, p = 0.003) and WM (HR 0.11, 95% CI 0.01 to 0.83, P = 0.03) but not for FL (P = 0.26). In DLBCL, gait speed explained significant variability in OS (R2 = 22.95%) compared with IPI score (R2 = 1.87%; p = 0.005) whereas it did not for WM compared with IPSSWM (R2 = 10.22% vs. 5.58%, p = 0.11) or FL compared with the FLIPI (R2= 12.21% vs. 8.10%, p = 0.35).
Conclusion: Gait speed may help to further refine the prediction of outcomes in patients with aggressive lymphomas beyond standard prognostic scores but may have less of an effect for indolent lymphomas. These data suggest that gait speed should be incorporated into the standard assessment of patients with aggressive lymphomas.
Buckstein:Takeda: Research Funding; Celgene: Consultancy, Honoraria, Research Funding. Soiffer:Mana therapeutic: Consultancy; Kiadis: Other: supervisory board; Juno, kiadis: Membership on an entity's Board of Directors or advisory committees, Other: DSMB; Gilead, Mana therapeutic, Cugene, Jazz: Consultancy; Cugene: Consultancy; Jazz: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal