Introduction: Oral novel therapeutics place a high financial burden on patients. A specialty pharmacy at Karmanos Cancer Institute (KCI) was established which streamlines prior authorization, determines patient cost-sharing, then automatically applies for additional financial assistance (through co-pay cards or foundation grant funding as needed) prior to setting final patient cost-sharing and drug delivery. We evaluated patterns of cost and need for additional funding since this program was established.
Methods: We used the KCI Specialty Pharmacy dataset for a retrospective review of patients who received prescriptions for hematologic malignancies between March 2018 - May 2019. Oral therapeutics >$10,000/month average wholesale price were considered high cost. We evaluated patients by drug prescribed and insurance type (Medicare, Medicaid, Private) and gathered information on insurer cost, final patient cost-sharing, cost covered by foundation grant assistance (if needed), and cost covered by manufacturer co-pay cards (if needed). We also calculated time in days from prescription written date to date of prior authorization, as well as prescription written date to date of delivery to the patient for all new first-time prescriptions.
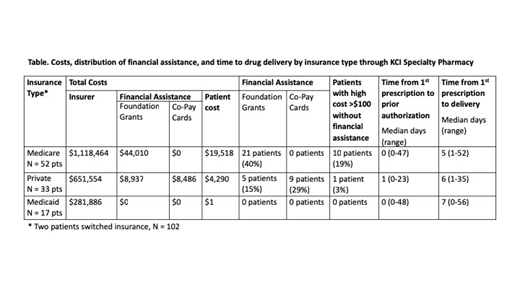
Results: 214 prescriptions among 100 patients were available for analysis. 2 of these patients switched insurance types. Drugs that were evaluated included imatinib, dasatinib, bosutinib, nilotinib, ponatinib, ruloxitinib, venetoclax, acalabrutinib, ibrutinib, ixazomib, midostaurin, gilteritinib, everolimus (for relapsed Hodgkin lymphoma), vorinostat, and enasidenib. The majority of patients had Medicare +/- supplemental insurance (52%), followed by private insurance (33%), and Medicaid (17%). Among all patients, 35% required additional financial assistance (for 75 claims). Most of these were through foundation grant funding (26% of all patients, 59 claims) and the remaining through manufacturer co-pay cards (9% of all patients, 16 claims). Medicaid patients did not require additional financial aid and have low cost-sharing given cost-sharing subsidies provided by Medicaid. Most of the patients requiring financial assistance were Medicare patients receiving foundation grant funding (Table). There were 10% of patients who did not receive additional assistance, but had high cost-sharing exceeding $100/prescription (range $295-$3514). Claims costs for all prescriptions totaled just over $2,000,000. The majority of the cost was paid by insurers with more than half covered by Medicare, ~$52,950 paid by foundation grant assistance, ~$8,486 paid by manufacturer co-pay cards, and $23,818 by patient cost-sharing. There were 105 first-time prescriptions to evaluate. When comparing the times required for prior authorization and delivery of drugs to patients, median times were similar by insurance type (Table), and most prescriptions received prior authorization approval within 1 day and were delivered within 7 days.
Conclusions: Financial assistance was needed for 35% of all patients on novel therapeutics, mostly through foundation grant assistance. Medicare covered half of total 2 million dollar cost. Medicare patients bear the most burden, with 40% requiring foundation grant assistance, and 19% acquiring high co-pays. The KCI Specialty Pharmacy attained a total of ~$61,433 in financial assistance, and provided an efficient process for fast authorization and drug delivery which did not vary by insurance type or need for grants.
Smith:Genentech Advisory Council: Other: Pharmacy Consultant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal