Background
Variation in the gastrointestinal microbiota after hematopoietic cell transplantation (HCT) has been associated with acute graft-versus-host disease (aGVHD). The significant immunosuppression associated with HCT leads to frequent broad-spectrum antibiotic exposures that in turn drive host microbiota composition. We sought to explore the association of different antipseudomonal antibiotic classes, commonly administered as empiric therapy for neutropenic fever, with subsequent aGVHD-risk in a large, multicenter cohort of children undergoing HCT for acute leukemia. We hypothesized that antibiotic classes that retain broad anti-anaerobic activity would increase aGVHD due to the greater potential impact of these agents on the microbiota.
Methods
Children 1-21 years old who underwent first HCT for acute leukemia from 2004 to 2017 were identified in 2 databases: CIBMTR, an observational database with demographic, transplant and outcomes information, and PHIS, an administrative database with resource utilization data from freestanding children's hospitals. Patients were then merged based on date of birth, date of transplant, sex and disease.
The outcome was grade 2-4 aGVHD by day +100. The primary exposures were 3 distinct classes of antibiotics commonly used for empiric therapy: (1) antipseudomonal cephalosporins, (2) antipseudomonal penicillins and (3) carbapenems. They were captured as days of therapy from conditioning start to day +7, and classified as no, low (1-3 days), or high (>3 days) exposure.
Logistic regression was applied to evaluate the association between aGVHD and each exposure, controlling for exposure to the other two classes. For the subset of patients with data on date of GVHD onset, a time to event analysis was performed considering death without GVHD as a competing event. For both analyses, we constructed multivariable models that were informed by a directed acyclic graph and included covariates representing demographics, transplant characteristics and GVHD risk factors associated with both exposure and outcome. The adjusted models also included exposure to other antibiotics within the same window, captured as fluoroquinolones, intravenous vancomycin and other adjunctive antibiotics, with and without anti-anaerobic activity. Generalized estimating equations with robust variance estimates were employed to account for clustering at the hospital level.
Results
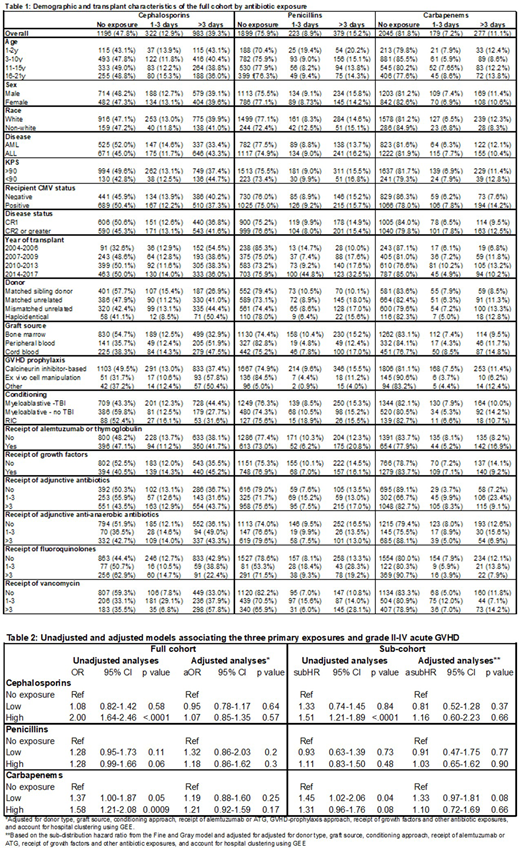
The assembled cohort included 2,501 patients at 35 hospitals. One-third of patients (36.6%) developed aGVHD, 4.4% died without GVHD and no patients were lost to follow-up. The proportion of patients exposed to at least 1 day of an antipseudomonal cephalosporin was 52.2%, but was lower for antipseudomonal penicillins (24.1%) and carbapenems (18.2%). Table 1 shows patient characteristics by exposure to the antibiotic classes of interest.
The unadjusted and adjusted associations between the three antibiotic classes and aGVHD are shown in table 2. In the unadjusted model, high exposure to cephalosporins and carbapenems was statistically associated with increased aGVHD risk. For antipseudomonal penicillins, the direction of association was the same but not statistically significant. After adjustment, most point estimates reverted towards the null.
The time to event analysis included 1,146 patients that were similar to the overall cohort with a similar incidence of aGVHD (35.5%) diagnosed a median of 28 (range: 8-100) days after HCT. This group had a higher proportion of mismatched donors (40.9 vs 30.2%), cord blood transplants (40.0 vs 23.5%) and receipt of growth factors (50.5% vs 38.9%). Table 2 also shows the unadjusted and adjusted associations for this analysis. As above, the unadjusted point estimates of association between cephalosporins and carbapenems and aGVHD were suggestive of an association but reverted towards the null with adjustment.
Conclusions
After controlling for other antibiotic exposures and GHVD-risk factors, there was not a statistically significant association between antibiotic exposure and aGVHD for any of three antibiotic classes commonly used for empiric therapy. However, the adjusted point estimates suggest exposure to carbapenems may confer some additional aGHVD risk. Further exploration of different exposure windows is planned to understand if the identified associations change with capture of earlier or later antibiotic exposures.
Jagasia:Kadmon: Consultancy; Incyte: Consultancy; Janssen: Research Funding. MacMillan:Alpine Immune Sciences: Consultancy; Angiocrine: Membership on an entity's Board of Directors or advisory committees; Incyte: Consultancy; Equillium: Membership on an entity's Board of Directors or advisory committees. Fisher:Pfizer: Research Funding; Astellas: Other: Data Safety Monitoring Board Chair for an antifungal study; Merck: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal