Introduction
Survival of hemato oncologic patients has significantly improved in the last 50 years due to more intensive treatments and directed therapies. This has led to a paradigm shift focused not only in achieving cure but also addressing survivors' complications such as treatment toxicities and second malignancies. Cardiac toxicity is one of the most frequent long-term complications after cancer treatment leading to a significant burden in morbidity and mortality. Anthracyclines are type 1 cardiotoxic drugs. Risk of cardiotoxicity depends on patient characteristics and drug combinations as well as anthracyclines cumulative doses. Treatment of many hematologic malignancies often includes anthracyclines. Cardiac toxicity may limit oncologic treatment along with a negative impact on functional prognosis of survivors. Cardio oncology is an emerging field aimed at prophylaxis, early detection and proper treatment in order to improve quality of life in cancer survivors. This is the first Uruguayan experience in the implementation of a cardio oncology protocol.
Methods
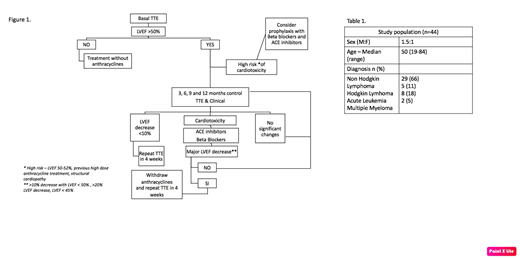
This is a prospective interventional study conducted by a multidisciplinary team formed by hematologists and cardiologists. Inclusion criteria were patients older than 18 years old with hematologic malignancies who received anthracycline treatment between march 2017 and march 2019, treated at our institution. All patients gave their informed consent. This protocol was approved by our institution Ethical Committee. Patients who entered the protocol were followed at the Cardio Oncology Unit. Trans thoracic echocardiogram (TTE) were performed using the same equipment and by experimented operators. Left ventricular ejection fraction (LVEF) by Simpson and Global Longitudinal Strain (GLS) were measured. Figure 1 shows the algorithm used. We defined cardiotoxicity as the decrease of LVEF greater than 10% (relative to baseline LVEF) to a threshold inferior to 53%; or a relative reduction of GLS greater than 15%.
Results
We created a Cardio Oncology Unit (COU) at our institution with hematologists and cardiologists. Forty-four patients were included (table 1). Protocol compliance was 70%. Seven percent (3/44) of patients presented structural cardiopathy and 20% (9/44) were defined as high risk (figure 1). Cardiotoxicity was diagnosed in 16% (7/44) of patients. The diagnosis was made using LVEF decrease in every case, no patient was diagnosed based on GLS. Mean time of onset was 3 months (1-6). Mean doxorubicin dose was 115 mg/m2 (50-200). Four of the patients were asymptomatic and 3 presented with heart failure. Two patients required suspension of anthracyclines due to cardiotoxicity. Six of the 7 patients diagnosed with cardiotoxicity were treated with Beta blockers and ACE inhibitors and treatment was well tolerated. Of these patients, two died due to their oncologic disease, three improved their LVEF, one maintained the LVEF stable in spite of continuing on anthracyclines. Structural cardiopathy was associated with greater risk of cardiotoxicity (p=0.013).
Conclusions
We present the results of the implementation of a Cardio Oncology prospective protocol at our institution. The incidence of cardiotoxicity evidenced was greater than expected according to anthracycline used doses, with early onset during treatment. We identified structural cardiopathy as a risk factor for cardiotoxicity. Our results highlight the relevance of cardiologic follow up in patients receiving anthracyclines and makes us question whether prophylaxis would be beneficial for high risk patients. We strongly believe that cardiotoxicity is a major problem for hemato oncologic patients, and that a multidisciplinary approach with health care protocols is the best way to address it.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal