Background
Sickle cell disease (SCD) is a progressively debilitating monogenic disease characterized by unpredictable, acute, life-threatening episodes and chronic complications such as hemolytic anemia and end-organ damage. It presents with a range of severity resulting in significant morbidity, poor quality of life, and early mortality. Real-world data on treatments and clinical outcomes for patients (pts) with SCD are limited, particularly in the community clinical care setting. The objectives of this retrospective real-world study were to characterize clinical manifestations and management of pts with SCD treated at the Foundation for Sickle Cell Disease Research (FSCDR).
Methods
A retrospective longitudinal analysis of an electronic health records (EHR) database from the FSCDR, which captured laboratory testing, treatments, and records on outpatient, emergency, and inpatient visits, was conducted. All unique pts with SCD assigned a medical record number in the EHR (N=172) were considered. Data from external records were manually entered into the EHR to supplement the EHR database. To address limitations of a real-world database, medical records for all pts included were manually reviewed and validation was performed on 10% of the sample. Pt demographics, clinical characteristics, hydroxyurea (HU) treatment (as captured by prescriptions and usage notes), administration of red blood cell transfusions, vaso-occlusive crisis (VOC) events and acute chest syndrome (ACS) (based on physician assessment) were described. Annual VOC rates were summarized by dividing the number of events by the total follow-up duration in years.
Results
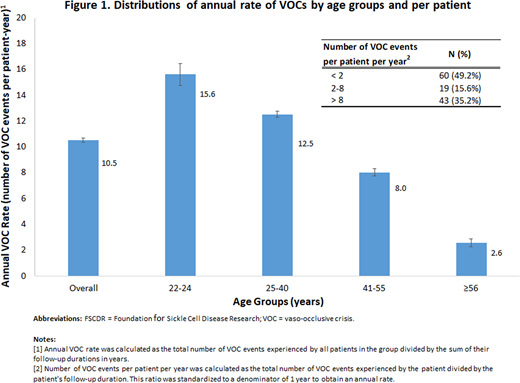
In total, 122 pts with SCD were included. Twenty-three pts were excluded as they were not actively seeking care and/or had no relevant clinical data from 01/01/15-07/19/19. Data for 27 pts <22 years of age were unavailable at time of analysis (results of this cohort will be included in the presentation). Among all pts, 76 (62.3%) were female and 118 (96.7%) were Black or African American. The mean age at time of analysis was 39.1 (standard deviation [SD] 12.3) years with 9 (7.4%) 22-24 year-olds, 67 (54.9%) 25-40 year-olds, 35 (28.7%) 41-55 year-olds, and 11 (9.0%) ≥ 56 year-olds. The most common genotypes were HbSS (77.0%) and HbSC (17.2%). Over a mean follow-up period of 2.9 (interquartile range: 2.0, 4.4) years, 27 (22.1%) pts were treated with HU and 66 (54.1%) pts received transfusions, of which 1 (1.5%) pt chronically received episodic transfusions (i.e., continuous monthly transfusions for ≥ 6 months). The mean total hemoglobin (Hb) was 8.3 (SD 1.7) for HbSS pts and 10.9 (SD 1.5) for HbSC pts. Among pts who never received HU or transfusions during follow-up, mean Hb was 9.4 (SD 1.7) for HbSS pts and 11.4 (SD 1.6) for HbSC pts. Among pts who ever received HU or transfusions, mean Hb was 7.7 (SD 1.3) for HbSS pts and 10.3 (SD 1.1) for HbSC pts. Eleven (9.0%) pts had ≥ 1 ACS whereas 97 (79.5%) pts had ≥ 1 VOC event. ACS and VOC events occurred mostly in pts 25-55 years of age (ACS: 9 [81.8%] pts aged 25-40 years and 2 [18.2%] pts aged 41-55 years; VOC: 54 [55.7%] pts aged 25-40 years and 29 [29.9%] pts aged 41-55 years). Annual rates of VOC are described in Figure 1.
Conclusions
This is one of the first studies to describe clinical characteristics and management of pts with SCD in a community practice setting. Higher Hb levels among pts who never vs ever received HU or transfusions during follow-up may be a reflection of who were selected for treatment and additional studies to take into account timing of treatment and Hb assessments and confounding factors need to be conducted. The study found high VOC rates particularly among pts aged ≤ 40 years. Lower VOC rates among older pts do not necessarily indicate less severe disease. One potential reason for lower VOC rates among older pts with SCD is that cumulative exposure to ischemia-related tissue injury and resulting end organ damage may decrease VOC-related pain over time. Further investigation to elucidate the rate of VOC decline observed in older pts is needed, including looking at underlying health and end organ damage. While limitations are inherent in real-world studies, these findings underlie the ability to and importance of studying SCD management and clinical outcomes in community care settings. This study highlights the clinical burden of SCD and possibly higher than expected unmet need in this community setting.
Bronté-Hall:bluebird bio: Research Funding. Huynh:bluebird bio: Research Funding. Puri-Sharma:bluebird bio: Employment. Chang:bluebird bio: Research Funding. Chawla:bluebird bio: Employment. Signorovitch:bluebird bio: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal