Objectives: Many tyrosine kinase inhibitors (TKIs) are approved for treating the chronic phase of chronic myeloid leukemia (CML-CP). This study aims at identifying the optimal upfront TKI treatment strategy; considering cost-effectiveness for CML patients from Qatar healthcare system perspective. Evaluated strategies included the newer generation TKIs; dasatinib 100 mg once daily and nilotinib 300mg twice daily. We evaluated both treatments considering their molecular and cytogenetic response outcomes at 12 months follow up as well their respective acquisition costs.
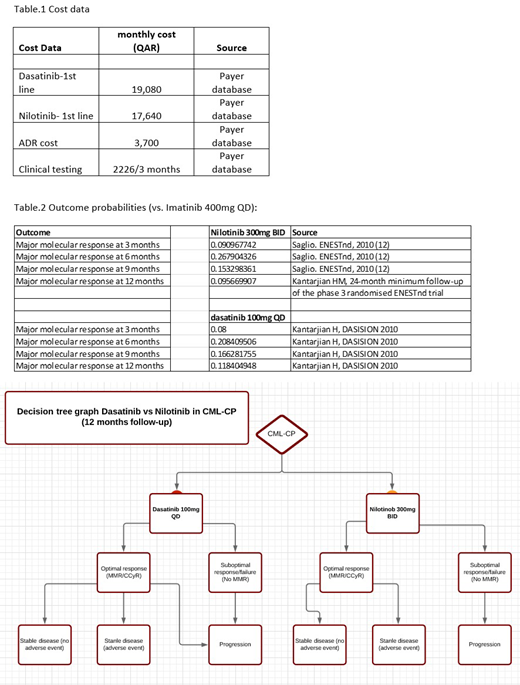
Methods: A decision tree model was developed linking clinical effectiveness (defined as major molecular response MMR and/or complete cytogenetic response CCyR), utility, and cost data over a 12-months period. The choice of 12 months period is due to the evidence that the degree of short-term molecular and cytogenetic responses at certain follow- up times is correlated with CML prognosis. Patients who achieve a CCyR are shown to have high remission rates as well overall survival (OS) rates. Patients with newly diagnosed CML are adopted from Qatar Cancer Registry.The probability of primary clinical outcome is calculated from DASISON (dasatinib) and ENESTnd (nilotinib) trials. Direct healthcare costs were derived from the national healthcare payer system, whereas ADR data were derived from local incident reporting system.
Results: In the first-line treatments of CML patients, with greater MMR (39% nilotinib vs 12% dasatinib) and CCyR (24% nilotinib vs 16% dastinib) response outcomes, and more adverse drug reactions (ADR) than dasatinib (13.3% vs 4%), nilotinib use is more cost effective with annual costs (QAR 232,102) and after 12 months follow up. Despite the lower acquisition annual cost of dasatinib (QAR 217,125), the incremental cost effectiveness ratio (ICER) of nilotinib versus dasatinib per MMR/CCyR achieved was 56,506 QAR per year. There were no cases in both arms that progressed to accelerated or blast phase. At a threshold of 3 times GDP per capita of Qatar and according to WHO recommendation, the nilotinib use is still cost-effective.
Limitations: For the surrogate outcome, we only consider the percentage of patients with or without MMR / CCyR response at 12 months. Nevertheless, we do not consider the depth and the duration of the MMR or CCyR.
Conclusions: Upfront therapy of CML-CP patients by nilotinib plan appears to be more cost-effective than dasatinib. Although local real-life data for the effectiveness of these drugs are still warranted. The results of this study implying that nilotinib would be advantageous as first-line treatment for CML-CP patients from Qatar healthcare system perspective.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal