Introduction: Despite the manifold symptoms that women with inherited bleeding disorders may experience, no study has specifically sought to understand the lived experiences of these women, nor the barriers to care that they may face. Indeed, the literature on this topic remains sparse. A MEDLINE search assessing literature on access to care for women with inherited bleeding disorders yielded 526 abstracts; of these, only a small subset (N=12) focused on women's health, and less (N=2) made any note of potential barriers to care. Given the lack of data on this subject to date, the objective of this qualitative descriptive study was to understand women's lived experiences with inherited bleeding disorders, and their perceptions around access to care.
Methods: A semi-structured qualitative interview guide was developed in conjunction with experienced hematologists (MS and RW), patient advocates from the Canadian Hemophilia Society (CHS; PW and DP), and a qualitative research expert (KD). Inclusion criteria for study enrollment included age ≥ 18 years old, English-speaking, and confirmed diagnosis of an inherited bleeding disorder. Women were recruited across Canada through identification by treating healthcare providers and study members of the CHS. They were then consented for telephone interview by SA. Interviews were transcribed verbatim, and analyzed using descriptive thematic analysis on NVIVO software. A random selection of interviews was coded by 2 team members (SA, KD) to ensure similar data interpretation.
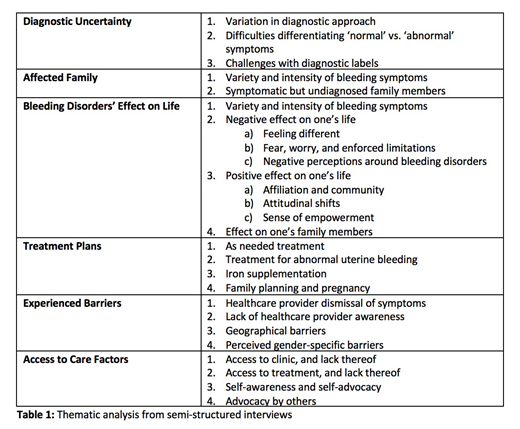
Results: Ten interviews with women with bleeding disorders were completed. Ages ranged from 24-70, and diagnoses included hemophilia B carriership (N=2), hemophilia A carriership (N=2), von Willebrand disease (N=2), disorders of platelet function (N=3) and dysfibrinogenemia (N=1). Common themes in the data included diagnostic uncertainty, affected family members, bleeding disorders' effect on life, the importance of treatment plans, experienced barriers, and access to care factors (Table 1). The most common barriers to care noted were healthcare provider dismissal of bleeding symptoms, lack of healthcare provider awareness, geographical barriers, and perceived barriers specific to women. Patients noted the importance of as-needed treatment, treatment for abnormal uterine bleeding, iron supplementation, and the need for family planning. They also highlighted the importance of access to clinic and treatment, and the need for self-advocacy.
Discussion: To our knowledge, this is the first study to assess lived experiences and barriers to care for women with inherited bleeding disorders. Our data indicates that women often feel dismissed by healthcare providers, and feel disempowered by not feeling understood or heard. These results may have implications for the ways in which healthcare providers communicate with their patients, particularly in the face of diagnostic uncertainty or predominantly gynecologic-related bleeding symptoms. By better understanding patients' lived experiences, providers may be able to provide more comprehensive, person-centered care.
Teitel:Novo Nordisk: Consultancy; Octapharma: Consultancy; CSL Behring: Consultancy; Pfizer: Consultancy, Research Funding; Bayer: Consultancy, Research Funding; Shire: Consultancy; BioMarin: Consultancy. Sholzberg:Novartis: Honoraria; Amgen: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal