Background
There was a limited improvement in the results of allogeneic hematopoietic stem cell transplantation (HSCT) in refractory leukemia over the last decades. The major reason of poor results is the relapse of the underlying malignancy. Thus the technologies to augment graft-versus-leukemia (GVL) effect is required for this group of patients. The preclinical study by Stokes et al. (British Journal of Haematology, 2016) indicated prolonged survival in the leukemia mouse model with substitution of posttransplantation cyclophosphamide (PTCy) with bendamustine (PTBenda). Also a small study evaluated the combination of PTCy and PTBenda in young patients and children (Katsanis E et al., 2018). We conducted the prospective study of postransplantation bendamustine as graft-versus-host-disease prophylaxis.
Methods
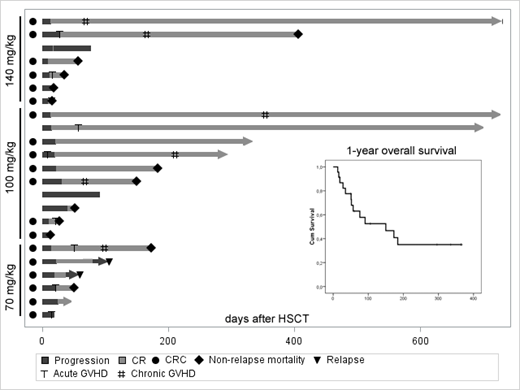
Single-center prospective dose-ranging de-escalation study (NCT02799147) evaluated safety and efficacy of PTBenda as GVHD prophylaxis. PTbenda was administered in doses 140, 100 and 70 mg/kg on days +3,+4. Myeloablative conditioning with fludarabine and busulfan was performed. First patients enrolled received single-agent PTbenda and subsequent- combination with other immunosuppressive agents. Inclusion criteria were acute myeloblstic (AML) or lymphoblstic leukemia (ALL) refractory to at least one induction course of chemotherapy or target therapy and more than 5% clonal blasts in the bone marrow. Twenty three patients were enrolled, 7 in the 140 mg/kg cohort, 10 in 100 mg/kg and 6 in 70 mg/kg, including 18 with AML and 5 with ALL. 35% of patients had primary refractory disease, and the rest - second or subsequent relapses, 61% had high-risk cytogenetics, 35% - complex karyotype, 17% - secondary AML, 30% - extramedulary disease. Median number of induction courses was 2 and 39% received target antibodies. Median number of blasts at transplant was 18% (range 6-97%). Two patients had matched related donor (MRD), 15 - unrelated (MUD), 6- haploidentical.
Results
Median follow-up was 10 months. The 140 mg/kg cohort was closed prematurely due to severe infectious complications. Ninety one percent of patients engrafted. Median time to engraftment was 16 days. Among the engrafted patients CR rate was 95%, and 67% had MRD(-) status. Relapse was documented in 10% of patients with CR. We have observed that PTBena induces a specific cytokine-release syndrome (CRC) with fever, vasculitis-like skin rush, oral mucositis, enteritis, hepatitis and pancreatitis. CNS signs, hypotension and respiratory failure were observed only in a few patients. CRC was observed in 78% of patients, including grade 1-2 in 17%, grade 3 in 26%, grade 4 in 22% and grade 5 in 3 patients. Median level of ferritin during CRC was 15 000 ng/ml and IL-6 levels were also increased (74 vs 8 ng/ml, p=0.036). Tocilizumab was administered to 13 patients and 10 responded. Classical grade II-IV GVHD was observed in 39% of pts and 60% of long-term survivors developed severe chronic GVHD. Non-relapse mortality was 48% with CRC, infectious complications and chronic GVHD as major causes. 1-year overall survival was 35%.
Conclusion
PTbenda even as a single agent has a significant potential to prevent acute, but not chronic GVHD. Moreover GVHD prophylaxis with PTbenda is a completely novel approach to induction of GVL, but optimal combination of immunosuppressive agents and supportive care should be determined to control the CRC and chronic GVHD. The optimal dosing regimen of PTbenda will be determined after enrollment in the last cohort will be completed.
Moiseev:Novartis: Consultancy, Honoraria, Other: Travel grants, Speakers Bureau; MSD: Other: Travel grants; Celgene: Consultancy, Other: Travel grants; BMS: Other: Travel grants; Takeda: Other: Travel grants; Pfizer: Other: Travel grants.
Bendamustine used for graft-versus-host disease prophylaxis.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal