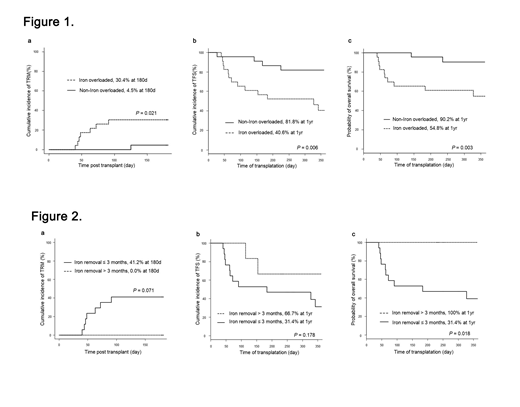
Abstract:The aim of this study was to evaluate the Impact of iron overload and iron removal therapy on the outcome of allogeneic hematopoietic stem cell transplantation (SCT) in patients with severe aplastic anemia (SAA). Forty-five transplant patients with SAA were retrospectively analyzed. Patients were divided into two groups according to whether there was iron overload or not: iron overload group (n=23) and non-iron overload group (n=22). The iron overload group had higher 1-year transplant-related mortality (TRM) (30.4% vs. 4.5%, P = 0.02), lower 1-year transfusion-free survival (TFS) (40.6% vs. 81.8%, P = 0.007) and lower 1-year overall survival (OS) (54.8% vs. 90.2%, P = 0.003) than the non-iron overload group. However, there was no significant difference in implantation rate, pre-engraftment syndrome (PES) and acute graft-versus-host disease (aGVHD, grade III-IV) between the two groups. Furthermore, the multivariate analysis revealed that iron overload was an independent risk factor affecting OS (HR = 36.88, P = 0.03). The patients in iron overload group were divided into two subgroups according to the time of iron removal using deferasirox 20mg/kg/d. Specifically, group A (n=17) was treated with deferasirox 20mg/kg/d for 3 months or less and group B (n=6) treated for more than 3 months. The results showed that group B had a lower one-year TRM (0% vs. 41.2% , P = 0.07), higher 1-year TFS (66.7% vs. 31.4%, P = 0.18) and higher 1-year OS (100% vs. 31.4% , P = 0.02) than group A. There were no significant difference in implantation rate, PES and aGVHD ( III-IV) between the two groups. In conclusion, the results indicate that iron overload before transplantation was associated with increased TRM and decreased OS, suggesting that iron overload was associated with worse transplantation outcomes. However, standardized iron removal therapy could reverse the adverse effects of iron overload on the outcomes of transplantation to a certain extent and improve the prognosis significantly.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal