Background
Allogeneic Stem Cell Transplantation (SCT) is potentially curative for many hematological diseases, however carries a high risk of mortality and morbidity. Multiple scoring systems has been developed to predict SCT outcomes and one of the more popular one id the Hematopoeitic Cell Transplantation - Co-Morbidity Index (HCT-CI). This study evaluates the value of HCT-CI score in predicting the outcomes of patients undergoing SCT at Princess Margaret Cancer Centre (PMCC). We also looked at the impact of the individual elements of HCT-CI in predicting SCT outcomes.
Methods
Two experienced physicians prospectively calculated the HCT-CI score for all patients transplanted at our center. Prospective calculation was performed during the patient's pre-transplant assessment before transplant admission using a pre-prepared form. All other patient and transplant characteristics were retrospectively collected from the EPR. Non-Relapse Mortality (NRM) and Overall survival (OS) were calculated to assess the prognostic power of the scores. This was correlated with the major SCT outcomes of Non-relapse mortality (NRM) and Overall survival (OS). Separately the impact of each components of HCT-CI was assessed in Univariate and multivariable analysis for NRM and OS.
Results
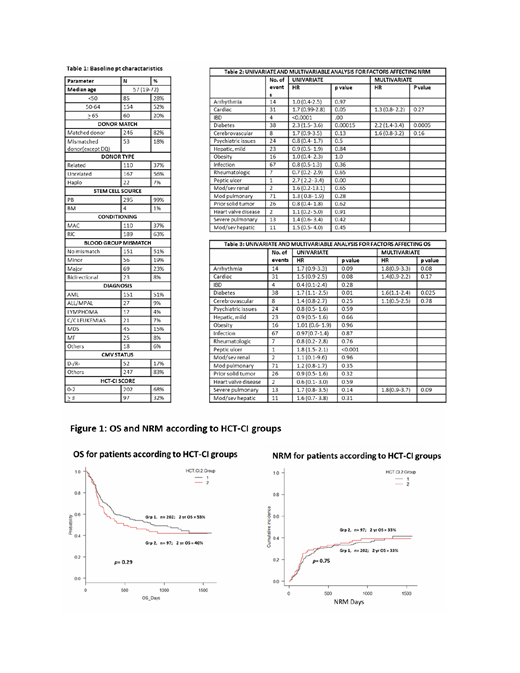
From August 2014 to April 2017, 299 patients underwent allogeneic HCT at the Princess Margaret Cancer Centre (PMCC), Toronto. Base line characteristics of the patients are shown in Table 1. HCT-CI scores were grouped as 0-2 as group 1 and ≥3 as group 2. Nearly two thirds belonged to group 1. (Table 1) The 2 year OS for the whole cohort was 51% (45%-56%) and NRM at 2 years was 25.1% (20%-31%). For the HCT-CI scores 0-2 vs ≥3, 2-year OS was 53% vs 46% respectively (p=0.29). The NRM at 2 years was 34% (29%-39%) for the whole cohort. For the HCT-CI scores 0-2 vs ≥3, 2-year NRM was 33% vs 35% respectively (p=0.75). (Figure 1)
Univariate analysis of the impact of the independent components of HCT-CI score on OS and NRM was done. A p value of 0.2 was taken as cut off for selection for multivariable analysis. For NRM, cardiac co-morbidity, Diabetes and cerebrovascular accident were considered for multivariable analysis, where as cardiac co-morbidity, diabetes, severe pulmonary comorbidity, arrythmia and cerebrovascular accident were considered for OS multivariable analysis. On multivariable analysis, diabetes was the only factor found independently impacting both NRM [HR 2.2 (95%CI 1.4-3.4), p=0.0005] and OS [HR 1.6 (95%CI 1.1-2.4), p=0.025].
Conclusion
HCT-CI was not found to predict OS or NRM accurately in our cohort of patients. Among the components of HCT-CI, diabetes was the only co-morbidity that significantly impacted both OS and NRM. Future prognostic scorings should incorporate only significant elements of comorbidities along with other transplant and disease related elements while developing prognostic scores.
Mattsson:Therakos: Honoraria; Celgene: Honoraria; Gilead: Honoraria. Michelis:CSL Behring: Other: Financial Support.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal