Introduction - Salvage chemotherapy followed by autologous hematopoietic cell transplantation (auto-HCT) is the standard-of-care for relapsed and refractory (R/R) diffuse large B cell lymphoma (DLBCL) patients. Eligibility is based on the presence of chemo-sensitive disease as defined by complete remission (CR) or partial remission (PR) according to FDG PET/CT study post salvage therapy. Patients achieving CR prior to auto-HCT have better prognosis than those undergoing it in PR. However, to this date, it is not clear whether one should struggle to achieve CR prior to auto-HCT or is PR after first salvage therapy good enough.
Aim - To evaluate the role of additional salvage regimen prior to autologous HCT in R/R DLBCL patients who achieved PR per FDG PET/CT following first salvage regimen.
Methods - We retrospectively reviewed the medical records of all patients who underwent auto-HCT for R/R DLBCL at three Israeli stem cell transplant centers between 2008 and 2018. Patients were identified based on the reports to the EBMT registry or according to the center's surveillance data.
We recorded and compared outcomes between patients who achieved PR after first salvage therapy and proceeded immediately to auto-HCT vs. patients who continued with additional salvage treatment (either the same or a different regimen) before auto-HCT. Outcomes were compared between these groups and between patients who achieved CR after first salvage and patients with chemo-refractory disease who proceeded to transplant.
Continuous variables were described as the mean, median, standard deviation and range of n observations. Categorical data were described with contingency tables including frequency and percent. Differences between the two groups of patients were examined by the Mann-Whitney test for continuous variables, and the two-tailed Fisher's exact test for categorical variables. Progression Free Survival (PFS) was defined as the time from autologous HCT to post transplant disease progression or to death from any cause, whichever occurred earlier. Overall survival (OS) was defined as the time from HCT until the date of subject death from any cause. The Kaplan-Meier method was used to estimate the distribution and median PFS and OS. Disease response and disease progression were assessed according to the Lugano criteria.
Results - Between the years 2008 - 2018 149 patients underwent auto-HCT for R/R DLBCL. After first salvage chemotherapy 81 patients (54%) achieved CR, 50 patients (33%) achieved PR and 18 (12%) had progressive disease (PD). Among the 50 patients achieving PR after first salvage, 30 patients (60%) proceeded immediately to transplant and 20 patients (40%) were treated with additional salvage treatment. There were no differences between the two groups in the characteristics of the patients, the disease and regimens being given (Table).
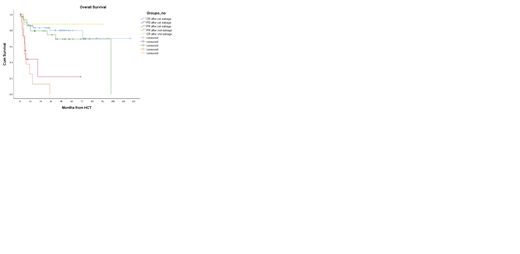
Median PFS was better for patients proceeding to HCT in PR compared to those who continued with additional salvage therapy in order to achieve CR (not reached vs. 12.5 months, p=.089). This was also true, with respect to OS (105 months vs. 35 months, p=.019). Interestingly, OS was comparable between patients who proceeded to transplant in CR or in PR after first salvage (Median not reached, vs. 105 months, p=0.245).
Among patients who received further salvage chemotherapy (either the same or a different regimen) and obtained CR before HCT (n=8), overall survival was comparable to those who achieved CR after first salvage (mean 84 months vs. 99 months, p=.35). Patients who were still in PR after second salvage had a dismal prognosis which was comparable to that of patients proceeding to HCT in progressive disease after first salvage (mean OS of 11 vs. 22 months, p=.24).
Conclusions - Albeit the small number of patients, our results do not support the administration of further salvage treatments in R/R DLBCL patients achieving PR after first salvage treatment in order to achieve pre-transplant CR.
Gurion:Roche: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal