Introduction:
Hematopoietic stem cell transplantation (HSCT) is a potentially curative or consolidative therapy for a large number of hematological diseases. Sexual dysfunction (SD) and abnormal level of the sexual hormone are common in patients after HSCT, which are usually caused by intensive myeloablative conditioning. The change of sexual hormone level and SD resulted in the poor quality of life in this population after transplantation. The current aims of this study were to determine: (i) the incidence rate of SD and the association with androgen post both autologous (auto) and allogeneic (allo) HSCT; (ii) multi-factors analysis between SD and clinical characteristics, primary diease, donor type, cGVHD, etc; (iii) the association of androgen with cGVHD and glucocorticoid (GC) therapy.
Methods:
From April 2010 to February 2019, a total of 126 (74 males and 52 females) patients with hematological diseases undergoing HSCT were enrolled in our study. The reason for the small sample of patients was that only 126 patients completed our Sexual Function Questionnaire. Controls were 108 healthy, age and gender matched persons came from Medical Examiniation Center of our hospital. Assessment indexes included clinical characteristics, donor type, GVHD incidence, sex hormone levels, and Sexual Functioning Questionnaire (SFQ). The SFQ was implemented by the team members of our research group through a telephone interview, email, paper letter, and WeChat. All of the information and privacy of each patient was strictly conserved.
Results:
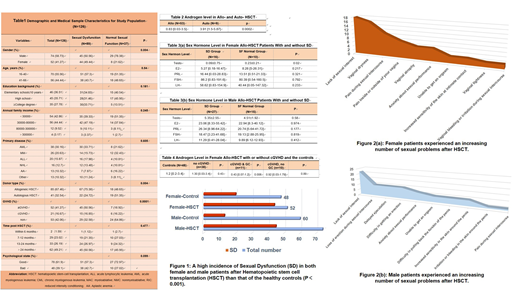
1. Clinical characteristics of the 126 patients who underwent HSCT were shown in Table 1. The median age of the patients was 38 years old (range 16-66) and the follow up after HSCT was from 6 months to 7 years. The predominant disease spectra were multiple myeloma (MM) and acute leukemia in auto- and allo-HSCT group, respectively. Our results showed a significant difference in gender (P<0.004), donor type (P<0.004), and GVHD development (P<0.0001), indicating a higher incidence of SD when we included these indicators into our analysis. There was no singficant difference of SD development in age, education background, annual family income, primary disease, time post HSCT, and phycological state.
2. Figure 1 showed a higher incidence of SD in both female and male patients after HSCT compared to the healthy controls (P<0.001). Most of them complained that they had trouble in normal sex life and sexual function had not yet recovered to the pre-transplantation level. Moreover, female patients exhibited much significantly decline in overall sexual function (OSD) than the male group (P<0.004). As depicted in the figure 2a and 2b, 54% female and 44% of male developed at least one physical sexual problem. Almost all of the female patients of childbearing age were infertility, and only a small number of young (< 30 years) male patients post transplantation could store fertility (data not shown).
3. From the foregoing data analysis, we confirmed that patients after allo-HSCT with or without GVHD usually acompanied with a higher incidence of SD compared to auto-HSCT group (Table 2). Female patients undergoing allo-HSCT who developed SD had a significantly lower level of androgen (P = 0.02, Table 3a), and that of the male patients was lower compared to healthy control with no significance (Table 3b). Female patients diagnosed with cGVHD had much lower adrongen level, especially in those received GC therapy (Table 4).
4. Although some young female patients had been given regular leuprolide injection every 28 days during their chemotherapy period or pre-transplantation, no significant difference was observed both in SD incidence and androgen level (P > 0.05, due to a small sample, data not shown here).
Conclusions:
Our results here indicated SD remained a major obstacle for patients to have a better quality of life after HSCT. We should pay more attention to the female patients because they might be at a higher risk to develop SD, especially in those underwent cGVHD and received GC therapy. To improve the sexual function for this population, more intervention methods including optimization of conditioning, better controlling of cGVHD, and reproductive function reservation might be helpful to reduce the incidence of SD. Finally, our study suggested that low androgen levels may contribute to SD and androgen replacement therapy might be a promising choice to improve OSD for patients undergoing HSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal