Introduction: Acute and chronic graft-versus-host-disease (GVHD) are common complications after allogeneic hematopoietic stem cell transplantation (HSCT). GVHD affecting the gastrointestinal tract (GI-GVHD) is a severe complication with symptoms affecting the entire GI-tract. Furthermore, treatment with anti-GI-GVHD drugs are associated with potential harmful effects. Despite this, 1/3 to 2/3of children undergoing endoscopy due to suspected GI-GVHD is on anti-GI-GVHD treatment at time of the procedure. The clinical condition and prognosisfor children with or without anti-GI-GVHD treatment pre-endoscopically, has not previously been evaluated.
The aims of the present study were to indentify clinical factors associated with initiation of anti-GI-GVHD treatment pre-endoscopically and to compare the two-year post-HSCT survival rate in those with ongoing versus non-ongoing anti-GI-GVHD treatment at time of endoscopy.
Material/methods: This was a retrospective cohort study including all Swedish paediatric HSCT centras.Hospital records and histopathology data were included for all children <18 years of age. HSCT was performed 2000-2012. Endoscopy and biopsy-sampling were done due to clincially suspected GI-GVHD within one year post-HSCT. The ongoing treatment group was defined as starting point of anti-GI-GVHD treatment ³one day pre-endoscopically. Survival rate was followed up to 2 years post HSCT.
The study was approved by the Swedish ethical committee.
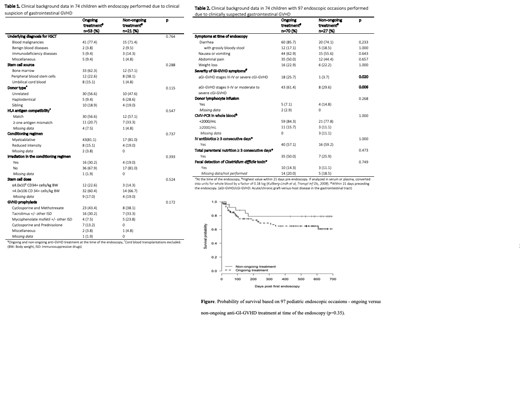
Results:HSCT-related background data are presented in Table 1.Seventy-four children with 97 endoscopic procedureswere included. Mean age at the time of HSCT was 9.0 (SD 5.5) years. From HSCT to endoscopy, the median duration was 81.0 days (IQR 37.0-153.0).
Anti-GI-GVHD treatment at time of the endoscopy was ongoing in 72% (70/97), and not ongoing in 28% (27/97). The median number of days with treatment before the endoscopy was 14.0 (IQR 5.5-35.0).
Histopathology confirmed GI-GVHD diagnosis was observed in 60% (42/70) in the ongoing-treatment group and 44% (12/27) in the non-ongoing-treatment group (p=0.18). The corresponding figure for normal or non-specific histopathological findings was 33% (23/70) and 48% (13/27) respectively (p=0.17).
Only higher symptom-based disease severity score (Table 1) was significantly more frequent in the ongoing treatment group (p=0.006). Furthermore, a pooled analysis was performedincluding background risk factors as HLA antigen mismatch, source of graft, graft containing > 4.0x106stem cells/kg or use of donor lymphocyte infusion pre-endoscopically. No significant differences were observed between the groups, regarding knowledge for the clinician of two or more risk factors versus having one or none (p=0.31).
The overall two-year post-HSCT survival rate for the entire study population was 64.9% . In a stratified proportional Cox regression analysisbased on the total number of endoscopies, 21/70 (30.0%) died within two years post-HSCT in the ongoing treatment group and 5/27 (18.5%) in the non-ongoing treatment group (Hazard ratio 1.63, 95% CI 0.59-4.54, p=0.35) (Figure 1). The causes of death differed significantly between the two groups, with relapse as a more frequent cause in the non-ongoing-treatment group (p=0.010), andnon-relapse mortality (NRM) in the ongoing treatment group (p=0.010). Nineteen children died due to NRM, nine due to infections, seven due to GVHD (all from the ongoing treatment group), three children died due to EBV-associated lymphoma (two in the ongoing treatment group).
Conclusions: We can conclude that, the more severely sick the child is, measured by severity of GI-GVHD symptoms, the more likely it is for the clinician to initiate anti-GVHD-treatment before endoscopy has been performed. Still, confirmed histopathological diagnosis was only found in 60 percent of the treated children. . The fact that GI-GVHD was only confirmed in 60 and 44 % respectively in the two groups, suggests that the non-specific symptoms of GI-GVHD may mislead the clinician to non-correctly start or not to start anti-GI-GVHD treatment, before a correct diagnosis. Finally, we found a substantial burden of NRM in the ongoing treatment group, dominated by infectious, partly an expected finding. However, if these findings are influenced by non-correctly initation of anti-GI-GVHD treatment pre-endoscopically, needs to be clearified in further studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal