Haematopoietic stem cell transplantation (HSCT) typically involves manipulation or reconstitution of the immune system regardless of whether the cells are autologous or allogeneic. Consequently, there is a considerable risk of auto-reactive lymphocytes escaping central and peripheral immune tolerance, especially in a severely immune-depleted host, with subsequent development of new autoimmune diseases1. The mechanisms underlying this autoimmunity are still largely unknown. Autoimmune haemolytic anaemia (AIHA) is the most frequently reported autoimmune disease after stem cell transplant with an incidence of 1.3% to 4.4%2,3 in current literature. Potential reported risk factors have varied with different studies.
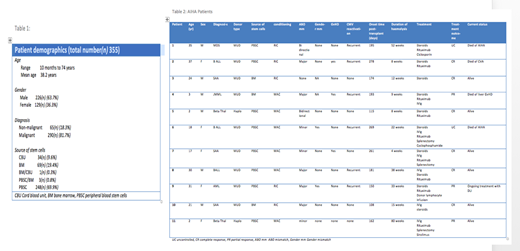
We considered some previously reported risk factors for AIHA (ABO antigen mismatch, myeloablative (MAC) versus reduced intensity conditioning (RIC), matched sibling donor versus unrelated or haplo-matched donor, concurrent graft versus host disease (GvHD), Gender mismatch and CMV reactivation status) in 355 patients who underwent haematopoietic stem cell transplantation at our centre during the period October 2012 to October 2018. Patients who received autologous stem cells were excluded. Patient demographics are shown in Table 1.
Results:
Eleven out of 355 patients developed clinically and biochemically evident, direct antiglobulin test positive, AIHA (3.1% incidence). The median time to onset, from HSCT to AIHA, was 181 days. Details of AIHA patients are shown in table 2.
Out of 355 patients, 179 had ABO antigen mismatched stem cell transplant (24 bidirectional, 82 major and 73 minor mismatched). Ten out of these 179 patients (5.6%) developed AIHA after transplant (2 out of 24 (8.3%) in bi-directional, 5 out of 82(6.1%) in major, 3 out of 73 (4.1%) in minor ABO mismatch group). One out of 176 patients (0.6%) who received an ABO matched stem cell transplant developed AIHA. This made the higher risk of AIHA in patients receiving ABO mismatched stem cell transplant compared with ABO matched counterpart statistically significant (RR 9.83(95%CI 1.3-76.0),p value=0.028).
Six out of 106 patients (5.6%) developed AIHA in the MAC group and 5 out of 249(2.0%) in the RIC group. There was no statistically significant difference between MAC and RIC (p value=0.07).
One hundred patients in our study received stem cells from matched sibling donors and none of them had evidence of AIHA after successful transplantation. In contrast, 11 out of 255 (4.3%) patients who received stem cells from unrelated donor or haplo-identical donors developed AIHA after transplant. However, there was not enough data for this trend to be statistically significant (p value =0.11).
We also looked at the presence of concurrent GvHD as a possible risk factor for developing AIHA after transplant. Three out of 120 (2.5%) patients with GvHD and 8 out of 235 (3.4%) patients without GvHD developed AIHA. This was not statistically significant (p value=0.64).
Similarly, there was no statistically significant association of post-transplant AIHA with gender mismatched donor transplant (p value= 0.78) or CMV reactivation status (p value= 0.13).
Conclusion:
Autoimmune haemolytic anaemia after stem cell transplantation is poorly understood due to the complex process of lympho-depletion, immunosuppression, immune reconstitution and graft versus host effects during and after successful transplantation. Our data show that receiving stem cells from ABO mismatched donor is a strong risk factor for developing autoimmune haemolytic anaemia after transplant. Further understanding of immune mechanisms underlying autoimmunity after stem cell transplantation will help to reduce the incidence of AIHA and to improve the overall survival.
References:
1. Holbro A, Abinun M, Daikeler T, et al. Management of autoimmune diseases after haematopoietic stem cell transplantation. British Journal of Haematology. 2012;157, 281-290.
2. Sanz J, Arriaga F, Montesinos P, et al. Autoimmune hemolytic anemia following allogeneic hematopoietic stem cell transplantation in adult patients. Bone Marrow Transplant. 2007;39(9):555-561.
3. Wang M, Wang W, Abeywardane A, et al. Autoimmune hemolytic anemia after allogeneic hematopoietic stem cell transplantation: analysis of 533 adult patients who underwent transplantation at King's College Hospital. Biol Blood Marrow Transplant. 2015; 21(1):60-66.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal