INTRODUCTION:
Graft-versus-host disease (GVHD) is a major complication of allogeneic hematopoietic cell transplant (HCT) resulting in significant morbidity and mortality. The combination of tacrolimus and sirolimus (TAC/SIR) has emerged as a GVHD prophylaxis platform preferred by many institutions given its association with rapid engraftment and acceptable transplant-related toxicity. However, overlapping toxicities between the two drugs can lead to intolerance and premature discontinuation in some patients. There is limited literature describing outcomes and subsequent management of such patients. The goal of this study is to investigate the clinical outcomes of patients becoming intolerant to the combination of TAC/SIR prophylaxis.
METHODS:
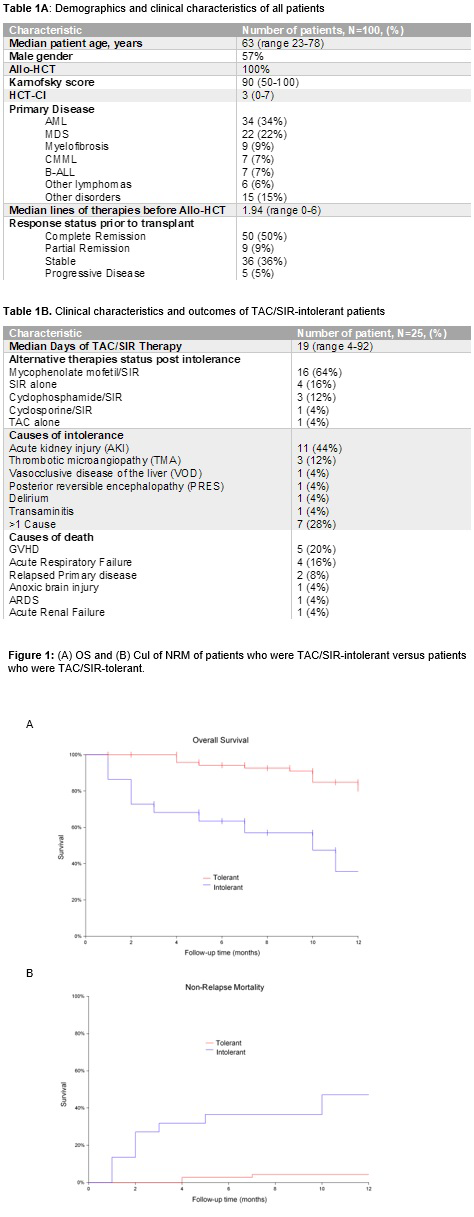
We retrospectively evaluated consecutive adult patients (n=100) at the Moffitt Cancer Center who received allogeneic HCT with TAC/SIR for GVHD prophylaxis in 2018. TAC/SIR intolerance was defined as discontinuation due to the toxicity of either TAC or SIR before post-transplant day 100. Survival analyses were estimated from the time of transplant with the Kaplan-Meier method and compared using the log-rank test. Patients intolerant of this prophylaxis regimen were compared to patients who completed >100 days of therapy, using Mann-Whitney U test for continuous variables and Pearson Chi-square tests for categorical variables. All statistical analyses were performed using SPSS v25 and NCSS v11.
RESULTS:
Demographics and clinical characteristics of all patients are summarized in Table 1A. TAC/SIR intolerance occurred in 25% (24 discontinued TAC, 1 discontinued SIR) of patients at a median duration of therapy of 19 days (range 4-92). The most common TAC/SIR toxicity (Table 1B) was acute kidney injury (AKI, n=11, 44%), followed by thrombotic microangiopathy (TMA, n=3, 12%). Baseline metabolic and clinical variables including creatinine, liver function, and conditioning intensity were not predictive of TAC-SIR intolerance. At a median follow-up of 10 months, the median overall survival (OS) for patients intolerant of TAC/SIR was 10 months versus was not reached for the patients without intolerance (HR 5.42; 95% CI 1.71-17.14; p<0.001). The 1-year PFS was 16% (95% CI 0% - 42%) vs 75% (95% CI 65% - 86%) and OS was 35% (95% CI 8% - 63%) vs. 79% (95% CI 68% - 90%) for patients who were TAC/SIR-intolerant compared to those who were TAC/SIR-tolerant (p<0.01) (Figure 1A). The cumulative incidence (CuI) of non-relapse mortality (NRM) at 1 year in patients intolerant of TAC/SIR was 47% (95% CI: 28% - 81%) and in patients tolerant of TAC/SIR was 4.4% (95% CI: 1.5% - 14%), (p<0.001). The Cul of relapse at 1 year was 45% (95% CI: 20% - 100%) in patients who were TAC/SIR-intolerant compared to 18% (95% CI: 10% - 30%) in patients who tolerated TAC/SIR (p=0.07) (figure 1B). Overall, 31 patients (31%) developed grade II-IV acute GVHD (aGVHD). The Cul of grade II-IV aGVHD at 100 days in patients who were TAC/SIR-intolerant was 29% (95% CI 15% - 58%) compared to 17% (95% CI 10% - 29%) in patients who tolerated TAC/SIR, (p=0.38). The Cul of cGVHD at 1 year in patients who were TAC/SIR-intolerant was 44% (95% CI: 25% - 79%) compared to 52% (95% CI: 40% - 68%) in patients who were TAC/SIR-tolerant (p=0.89).
CONCLUSIONS:
Outcomes for patients completing over 100 days of TAC/SIR for GVHD prophylaxis following allogeneic HCT are favorable. However, early intolerance of TAC/SIR GVHD prophylaxis occurred in 25% of allogeneic HCT in 2018 alone and predicted a poor prognosis with increased NRM and overall mortality, largely from drug-related toxicities. Notably, premature discontinuation of TAC/SIR did not contribute to higher subsequent risks of GVHD. Strategies to mitigate the risks of TAC/SIR toxicity are warranted. Future studies are also needed to identify the optimal GVHD prophylactic regimen for patients after TAC/SIR intolerance.
Nishihori:Novartis: Research Funding; Karyopharm: Research Funding. Bejanyan:Kiadis Pharma: Other: advisory board.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal