Objective: Invasive fungal disease (IFD) is a serious complication after allogeneic hematopoietic stem cell transplantation (HSCT). However, limited data is available on its clinical features after cord blood transplantation (CBT) for patients with hematological malignancies.
Method: We retrospectively reviewed 63 patients who underwent myeloablative CBT at our institution between July 2013 and June 2019 with a median follow-up of 14 months. Micafungin, Voriconzole or Posaconazole was used for IFD prophylaxis.
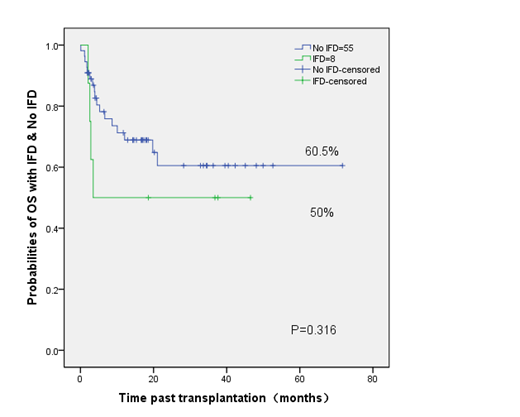
Results: Eight patients were identified as having an IFD, including 2 with proven IFD, 1 with probable IFD, and 5 with possible IFD. The most common prophylaxis regimen is micafungin (68.2%, 43/63). The incidence rate of IFD in the primary antifungal prophylaxis (PAP) and secondary antifungal prophylaxis (SAP) groups were 11.3% and 25% (P=0.488). The OS of day at +100, six months and +200 in the IFD and No IFD groups were 62.5% vs. 86.9% (P=0.1), 50 % vs.78.2% (P=0.07), and 50% vs.75.9% (P=0.094), respectively. The 3-year probabilities of overall survival (OS) in the IFD and No IFD groups were 50% and 60.5%, respectively (p=0.316). The incidence rate of Non-relapse Mortality in the IFD and No IFD groups were 42.9% and 30%, respectively (p=0.319).
Conclusion: Antifungal prophylaxis could help to reduce the incidence of IFD after CBT for patients with hematological malignancies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal