Background: Recent studies have demonstrated a prolonged progression-free survival (PFS) in CLL patients receiving ibrutinib-based regimes as upfront therapy. These studies, however, are limited in number and heterogeneous regarding patients' selection criteria, treatment combinations and schedules. Because of this, we conducted a meta-analysis of randomized clinical trials using ibrutinib as upfront treatment to evaluate the strength of the evidence and patients' subgroups who benefit the most of such treatment.
Materials & Methods: A systematic literature search was performed using PubMed to identify full length reports dealing with the randomized clinical trials (RCTs) of ibrutinib, used alone or in combination as upfront therapy of CLL prior to August 2nd, 2019. A complementary manual search of the ASH, EHA and ASCO conference proceedings was also performed. The search strategy used both Medical Subject Headings (MESH) terms and free text words to increase the sensitivity of the search. The electronic search yielded 4 full-text articles assessed for eligibility.
Results: In total 4 RCTs (i.e., RESONATE2, ALLIANCE, ILLUMINATE, ECOG-ACRIN) including 1574 untreated CLL patients compared head-to-head an ibrutinib-based regimen to CT or CIT. Inclusion criteria were either age 65 years or older or coexisting conditions for 1045 patients and age younger than 70 years in absence of coexisting conditions for 529 patients.
Among patients treated with an ibrutinib-based regimen, 318 received ibrutinib as single agent and 649 ibrutinib in association with anti-CD20 monoclonal antibodies (i.e., 536 ibrutinib + rituximab [R], 113 ibrutinib + obinotuzumab [Obino]). The CT or CIT control arms included 607 patients and consisted of chlorambucil (CLB)(n=133), CLB+Obino (n=116), bendamustine and R (BR) (n=183) and fludarabine, cyclophosphamide and R (FCR)(n=175).
All four studies included in the quantitative meta-analysis had enough data to assess PFS. Results indicate that treatment with ibrutinib-based regimens improved PFS compared with CT or CIT. The pooled HR for PFS in ibrutinib-treated patients was 0.331 (95% confidence interval [CI]: 0.272-0.403; P=0.000). The I2 statistic for heterogeneity (i.e. 0%; P=0.50) and Q values (i.e. 3.35) indicated a high level of homogeneity of results across studies. Of note, data were robust with no evidence of obvious publication bias (i.e., Funnel plot analysis indicate several missing studies that would bring p-value up to >0.05=156).
Overall survival (OS) was evaluated in 3 studies accounting for 1017 patients and revealed an HR of 0.289 (95% CI, 0.071-0.1175), with definite heterogeneity across studies (I2=82.7%; Q=11.6; P=0.003).
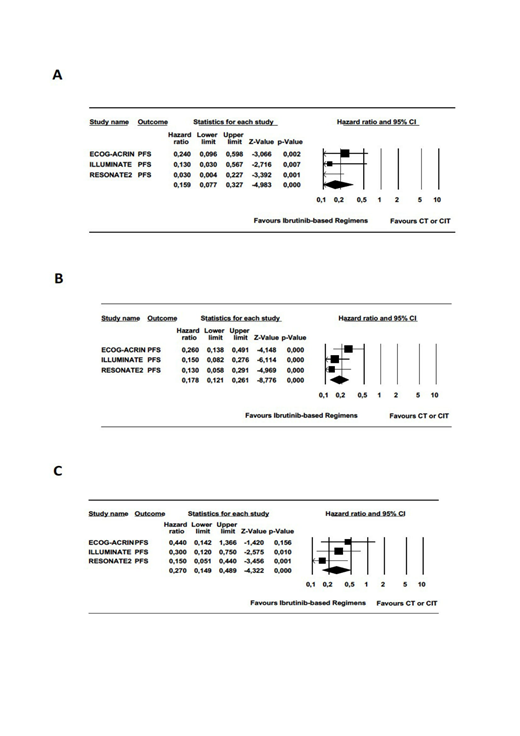
Next, we evaluated the magnitude of improvement in PFS obtained with ibrutinib-based regimens in patients with high-risk genetic features such as 11q deletion and unmutated IGHV status. Data for PFS by 11q deletion status, restricted to 3 studies (n=206), revealed a significantly lower risk of progression for 11q deleted patients treated with ibrutinib-based regimens (HR,0.159; 95% CI: 0.077-0.327; I2 = 42%; P=0.18; Q = 3.46) (Fig 1A). Of note, a lower risk of progression was observed in both patients with unmutated (n=522) (HR, 0.178; 95% CI, 0.121-0.261; p=.000; I2=11%; Q=2.21;P=0.32)(Fig 1B) and mutated IGHV (n= 287)(HR, 0.270;95% CI, 0.149-0.489; I2=0%; P=0.38;Q=1.91)(Fig 1B) who received ibrutinib in upfront. Despite slight differences of the HR values between patients with mutated and unmutated IGHV, interaction analysis suggests that the magnitude of PFS improvement is comparable in both groups (HR, 1.50; 95% CI, 0.74-3.04; P=0.87).
Conclusions This meta-analysis validates the notion that in comparison with CT or CIT ibrutinib-based regimens, given as upfront therapy, abrogate the negative impact of 11q deletion and unmutated IGHV on PFS. Even more, 11q deletion could be a favorable predictive biomarker for ibrutinib therapy. Because of design and selection criteria of studies included in this meta-analysis, some aspects such as the impact on response and its duration in patients with 17p deletion/TP53 mutations need further evaluation. Nonetheless, our results should inform updated algorithms of upfront CLL treatment.
Molica:Gilead, AbbVie, Jansen, Roche: Other: Advisory Board. Levato:Novartis: Honoraria; BMS: Honoraria; Incyte: Honoraria; Pfizer: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal