Background:
According to claims-based studies, a minority of MDS patients receive disease-modifying therapy. Unfortunately, these studies are limited by design in describing the shared decision-making process between MDS patients and their physicians in choosing supportive care, such as blood transfusions. Therefore, we surveyed and interviewed transfusion-dependent (TD) MDS patients and MDS physicians about the choice and use of supportive care, blood transfusions, and chemotherapy.
Methods:
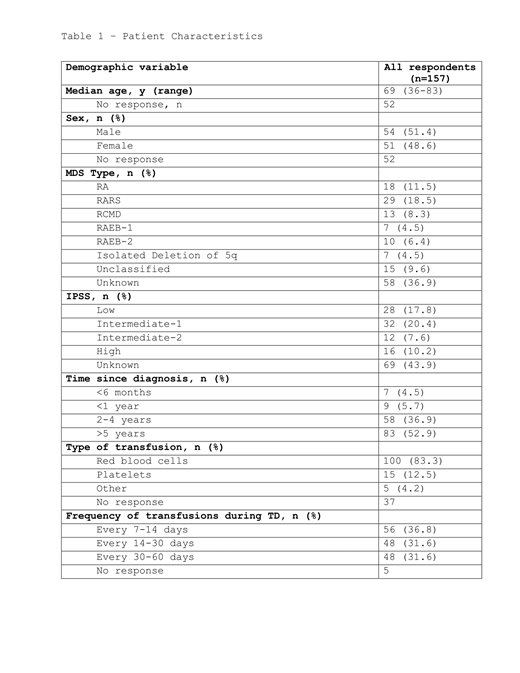
Nearly 300 TD-MDS patients and MDS physicians were surveyed or interviewed under an IRB exempt protocol (WIRB). Semi-structured interviews of 15 patients and 10 providers were conducted between July and December of 2018 to inform survey development. Patients and providers within the AAMDSIF database were then invited via email and social media to participate in anonymous surveys. Survey respondents were entered into a lottery to receive a $50 gift card. Each interviewed patient was offered a $25 gift card and each provider interviewee was offered a $50 gift card. Survey 1 queried MDS patients who self-reported they had been TD, defined as 2 or more blood transfusions within a 2-month timespan, at some time since 2014. Between September 2018 and February 2019, 157 TD-MDS patients responded. Primary variables of interest included patient age, sex, use of disease-modifying therapies, use of chelating agents, and frequency of blood transfusions. Survey 2 queried providers who regularly manage TD-MDS patients (n=109). Nominal and ordinal variables were tested for possible association by the Goodman-Kruskal tau statistic.
Results:
Demographics and baseline disease characteristics of TD-MDS patients are shown in Table 1. In brief, the patient cohort had a median age of 69 years (range, 36-83), male 51%, and a greater proportion of low and low-intermediate IPSS risk. Nearly half of patients were unaware of their IPSS risk group. The majority (57%) of patients were TD within the past 2 months of answering the survey. Two-thirds of patients received care from an MDS specialist. MDS providers practiced in academic medical centers (61%), community hematology/oncology specialty practices (17%), community urban hospitals (10%), community suburban hospitals (5%), and rural community hospitals (4%), with some providers practicing in multiple locations. On a monthly basis, the majority (85%) of providers cared for up to 10 patients with TD-MDS. The highest ranked patient concerns about blood transfusions were transfusion reaction and iron overload. Concern for the more common risk of bacterial infection ranked 5th and was least often selected as the most important concern to patients. Approximately half of patients reported use of an iron chelating agent. On qualitative interview, most patients did not recall a discussion with their physician regarding the risks of blood transfusions, despite providers reporting they regularly educate patients and ask for informed consent. Further, although 98% of patients visited their MDS care provider at least quarterly, 48% stated they had not discussed alternatives to blood transfusion with their provider. Many patients held the sentiment there was "no choice to be made" in receiving blood transfusions. While providers said blood transfusions as primary management of MDS was rare, they reported they would recommend transfusions as stand-alone therapy in settings of patient preference for supportive therapy only, failure of ESAs, patient desire for transfusion-only therapy, and older patient age. Most patients (65%) ranked their quality of life positively, with 6% ranking excellent. The majority (58%) of patients drove themselves to their transfusion clinic, and 54% of patients traveled greater than 10 miles to these visits. Older age significantly associated with higher transfusion frequency (G-Test = 31.318, χ2 df = 18, p-value = 0.02644), but not with use of disease-modifying therapy. The presence of comorbidities was not associated with either transfusion frequency or active therapy. No significant association was found between patient income and either transfusion frequency, BMT, or administration of HMAs.
Conclusions:
MDS patients and physicians hold differing perceptions about the choice to receive and risks of receiving blood transfusions. Appraisal and optimization of the informed consent process between TD-MDS patients and physicians are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal