Background: The TP5 gene is by far the most frequently mutated gene in human cancer. Some studies have shown that TP53 should be used as an independent prognostic biomarker in the prognostic stratification of myelodysplastic syndromes(MDS) and acute myeloid leukemia (AML). In this study, we want to explore the effects of different TP53 mutation status on clinical outcomes in AML and MDS.
Method and Results: We retrospectively collected and analyzed 51 patients with TP53 mutation from Jan 1st , 2015 to May 1st , 2019 in West China Hospital, Sichuan University, China. Among 51 patients, 27 patients were diagnosed as MDS,11 were diagnosed as AML. Then average age is 55.7(15-77). According to IPSS-R of MDS, there are 18 out of 27 patients in the high-risk and very high-risk groups, only 1 patient in the intermediate risk group and 8 patients lost follow up. 10 out of 11 AML patients were in the high risk group according to the NCCN guideline.
In our analysis, the incidences of complex karyotype and additional gene mutations were 86.67% and 36.84% in MDS and AML patients. AML evolution was 40.74% in MDS patients. The median follow-up time was 16 months (4-51 months) and the median overall survival was 7.61 months (range, 2-17 months). So far, 28.95% patients are still being treated, of which 9 have been treated with hypomethylating agents.
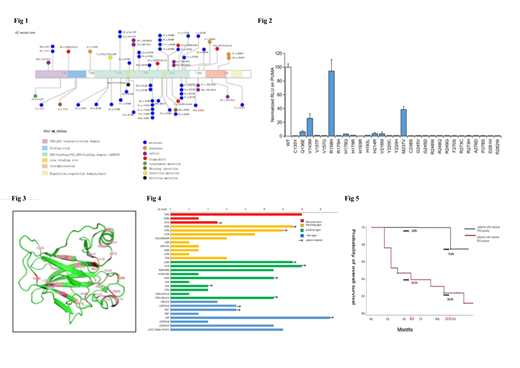
To compare the clinical outcome with different TP53 mutations status, firstly, we identified the mutation types and various mutants activity. We counted 62 TP53 mutations in 51 patients and marked their sites at the transcriptional level in Fig1 . Codons 248, 273, 175, 282, 245, and 249 are most common somatic mutations in TP53. Herein, the TP53 mutation hot spots found in 38 AML or MDS patients are clustered in the DNA-binding domain. Then we used the luciferase reporting system to test the p53 mutant activity with missense mutations in the DNA-binding domain as a transcription factor. The results in Fig2 showed that with the exception of R158H, M237V , V143M , Q136E and H178Q, almost all the other mutation types have no activity. And we demonstrated these TP53 hotspot mutations in the structure ( Figure 3). The overall survival time of patients with residual P53 mutant activity (except for the compound mutation) far exceeded the median overall survival(7.61months). For the other patients with mutants which almost completely lost the activity of p53 protein as a transcription factor, two patients were treated with hypomethylating agents followed by hematopoietic stem cell transplantation have survived for 14 and 11 months after diagnosis, respectively. As shown in Fig4 and Fig 5, we compared the OS of these two group patients with different P53 mutant activity and different function areas for 6 months and 12 months, respectively. The results showed that the patients with residual P53 activity survived better
Conclusion: Patients with different TP53 mutations do have different clinical outcomes. Patients with residual P53 mutant activity do respond better to treatment, and the final clinical outcome of patients who lose P53 activity completely is poor, but hypomethylating agents and hematopoietic stem cell transplantation can also ppropriately prolong survival time.
Legends to the figures
Figure1: 62 TP53 mutations in 51 patients with hematological neoplasms. The TP53 mutation hot spots found in 38 AML or MDS patients are clustered in the DNA-binding domain. There were 9 patients with multiple TP53 mutations. The black label represents somatic mutation, and the red label represents germline mutation. Missense mutations account for 61.70%(29/47) of all the TP53 mutations in 38 patients.
Figure 2: The p53 mutant activity with missense mutations in DNA binding domain tested by the luciferase reporting system. We compared the normalized RLU on PUMA of P53 mutant with wild type.
Figure 3: The structure of the p53 core domain bound to DNA. We marked the residues affected by the TP53 hotspot mutations . The deeper the red, the higher the mutation frequency and the more the mutation clustered
Figure 4 : The overall survival of 30 follow-up patients. We use a bar chart to show the clinical outcome(OS) of 30 patients with different mutation types and P53 structure affected by different p53 domains.
Figure 5 : The probability of overall survival of 30 follow-up patients. They are divided in two groups: patients with residual P53 activity VS patients with inactive P53 mutant.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal