Introduction: Pulmonary hypertension (PHT) is an emerging complication of myeloproliferative neoplasms (MPNs). The aim of this study was to determine the prevalence and risk factors of high echocardiographic probability of PHT according to 2015 The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) Guideline. The echocardiographic probability of PHT was assessed by peak tricuspid regurgitation velocity (TRV max) and echocardiographic signs suggesting PHT.
Methods: This was a cross-sectional study conducted in Chiang-Mai University Hospital during January 2019 and July 2019. Patients aged 18 years or older with Philadelphia chromosome negative MPNs including polycythemia vera (PV), essential thrombocythemia (ET), and myelofibrosis (MF) were eligible after obtaining informed consents. Patients who were known to have a preexisting PHT from any causes were excluded. All enrolled patients had an echocardiography performed by a cardiologist for evaluating the probability of PHT according to 2015 ESC/ERS guideline. Primary outcome of the study was the prevalence of MPNs patients who had high echocardiographic probability of PHT. Secondary outcomes were risk factor of high echocardiographic probability of PHT.
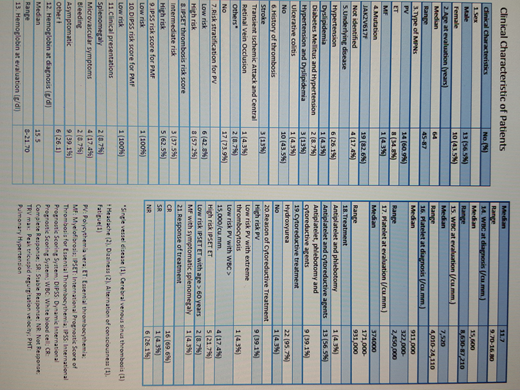
Results: A total of 23 patients with a median age of 64 years (range 45-87) were enrolled. There were 14 PV (60.9%), 8 ET (34.8%), 1 MF (4.3%) patients included. There were13 male patients (56.5%). The most common driver mutation was JAK2V617F mutation (19 patients, 82.6%). Common co-morbid diseases were hypertension (26.1%), combined hypertension and dyslipidemia (13%), and combined hypertension and diabetes (8.7%), respectively. The majority of patients (73.9%) did not have history of thrombosis. However, 57.2% and 62.5% of PV and ET patients were classified as high risk of thrombosis. Twenty two patients (95.6%) received both antiplatelets and cytoreductive agents with 9 patients (39.1%) also underwent phlebotomy. Hydroxyurea was only cytoreductive drug prescribed in this study. The median time from diagnosis to echocardiogram evaluation was 66 months (range 9-6,242 months). Median (range) hemoglobin was 11.7 g/dl (9.7-16.8), median white blood cells count was 7.5x109/L (4.0-24.1), and median platelet count was 374x109/L (171-931). No patient with high echocardiographic probability of PHT was detected. One patient (4.3%) patient had intermediate probability and 22 (95.7%) patients had low probability. The median value of TRV max was 2.42 m/s (range 1.93-2.90).
Conclusions: No MPNs patients (0/23) with high echocardiographic probability of PHT detected in this study. Further study with higher number of patients is warrant for determine the prevalence of PHT in Thai MPN patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal